Immunotherapy is showing great promise for treating cancer. But so far, this approach has been effective in only about 20% of all cancers. To advance those results, researchers are looking for new ways to mobilize the immune system to destroy tumors.
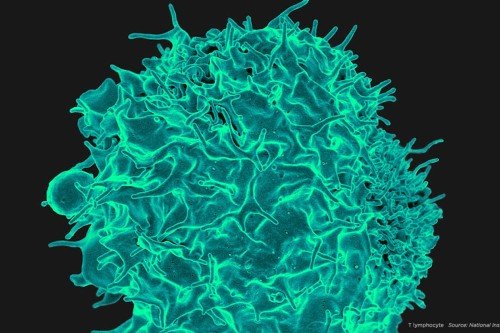
Most immunotherapy drugs act on one type of immune cells called T cells. Drugs called checkpoint inhibitors “release the brakes” on these cells, spurring them to mount an attack against a tumor. Researchers have learned that checkpoint inhibitors seem to work best in people whose tumors have been invaded by T cells — sensing some kind of threat from the cancer — before the treatment is started.
The problem is that most tumors don’t have many T cells in them. In order to design an immunotherapy that works on more people, researchers have been looking for additional immune cell types to rally against cancer.
Now, an MSK research team reports finding a promising candidate: a group of immune cells called innate lymphoid cells (ILCs). These cells are present in many different tissues and appear to have mild antitumor effects in their normal resting state. The researchers showed that activating ILCs with drugs mobilizes T cells to shrink pancreatic cancer tumors. This could be an important step, as pancreatic cancers have not responded to checkpoint inhibitor drugs.
“We think this is an important finding both for pancreatic cancer research and cancer immunotherapy overall,” says Vinod Balachandran, a surgeon-scientist affiliated with the David M. Rubenstein Center for Pancreatic Cancer Research and a member of the Parker Institute for Cancer Immunotherapy. “We are learning there are multiple ways to use the immune system to fight cancer. We think this is a sign that new immunotherapies are on the horizon.”
Dr. Balachandran made the discovery in collaboration with cancer immunologists Taha Merghoub and Jedd Wolchok of the Human Oncology and Pathogenesis Program. The finding is reported today in Nature.
Turning to Innate Immune Cells
ILCs are part of the body’s innate immune system where immune cells are programmed to put up an initial defense against infections and other threats, and further amplify the immune response by activating T cells. But ILCs were discovered only 10 years ago, so they have not been the focus of immunotherapy efforts. Now, innate immune cells are beginning to draw more interest from the cancer-research community. Dr. Balachandran and colleagues investigated if — and how — these cells played a role in the body’s response to cancer.
For the Nature study, the team looked in human pancreatic tumors to see if ILCs were present. They saw that a subtype of these cells called ILC2s were present in larger numbers in tumors compared with normal organs, suggesting they were responding to the tumors. The researchers also found that pancreatic cancer patients with more ILC2s in their tumors lived longer, suggesting ILC2s possibly had an anticancer function.
The team then tested if ILC2s could help control tumors in mice. Removing ILC2s caused pancreatic tumors to grow faster.
“We thought, if these cells have protective tendencies against cancer, maybe we can figure out ways to activate them,” Dr. Balachandran says.
Boosting Checkpoint Inhibition
ILC2s have receptors on their surface that control whether they multiply. The researchers found that dosing the ILC2s with a protein called interleukin 33 (IL-33) activated them, and caused both them and T cells to expand, which in turn caused tumors to shrink. IL-33 did not shrink tumors in mice that didn’t have ILC2s, proving the ILC2s were the key cells mediating the effects.
The research team then looked for ways to further amp up ILC2 antitumor activity. Checkpoint proteins on the surface of T cells act as brakes to prevent them from attacking the body’s own tissues. But this also limits the T cells’ antitumor activity. As ILC2s are related to T cells, Dr. Balachandran’s team wondered whether checkpoint proteins also acted as brakes on ILC2s.
They discovered that when activated by IL-33, ILC2s express an important checkpoint protein on their surface called PD-1. This has interesting immunotherapy implications: PD-1 is one of the most important brakes on T cells, yet PD-1-blocking checkpoint inhibitors have not worked well against pancreatic tumors. This suggested treating mice with IL-33 may make pancreatic tumors sensitive to PD-1-blocking checkpoint inhibitors.
When the researchers gave IL-33 plus a PD-1 inhibitor to the mice, the tumors shrank even more. Activating ILC2s by adding IL-33 appeared to be the key for PD-1 checkpoint inhibitors to work well against the mouse pancreatic tumors.
Dr. Balachandran and his team are currently working on developing a drug that can activate ILC2s in humans as the next step.
“This is a novel treatment that works together with one of the most successful immunotherapies we have today,” Dr. Balachandran says. “This could be a way to sensitize cancers that typically would not respond to PD-1 checkpoint inhibitors.”