This information will help you prepare for your cystogram at MSK.
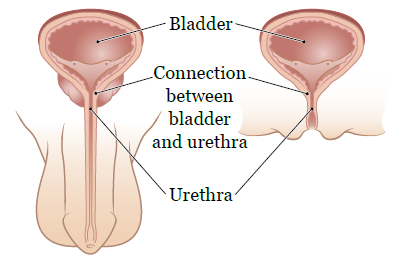
A cystogram is a type of imaging scan. It’s done to check for urine (pee) leaking from the connection between your urethra (the tube that carries urine from your bladder to outside your body) and the bladder (see Figure 1).
During your cystogram, your healthcare provider will put liquid contrast dye into your bladder through a urinary (Foley®) catheter (thin, flexible tube). Your healthcare provider will then take pictures of your urethra and bladder using an x-ray machine.
Before your procedure
Tell your healthcare provider if you:
- Are allergic to any medications or contrast dye.
- Are pregnant or if there’s any chance you’re pregnant.
You can take your usual medications on the morning of your cystogram. If you were prescribed antibiotics, please take them as prescribed. You can eat and drink as usual.
When you arrive for your cystogram, check in at the reception desk and have a seat in the waiting room. When it’s time for your procedure, a staff member will bring you to the procedure room. They will give you a hospital gown to change into.
During your procedure
If you don’t already have a urinary catheter, your healthcare provider will place one through your urethra, into your bladder.
The exam table will be adjusted so you’re lying flat. A lead cover will be placed on your neck. The cover will protect your thyroid gland from radiation from the x-ray machine. It may feel heavy, but you’ll be able to breathe and talk easily. You won’t wear a chest cover because it will block part of the picture.
When you’re ready, your healthcare provider will slowly put contrast dye into your bladder through the catheter. They will take x-ray images while they’re doing this to see if any contrast leaks from the connection between your urethra and bladder. You may feel fullness in your bladder or an urge to urinate (pee) while the contrast is being put into your bladder.
Once enough x-ray images are taken, the contrast will be slowly let out of your bladder through the catheter. More x-rays will be taken to make sure no contrast is left in your bladder.
Your cystogram should take 30 minutes or less.
After your procedure
At MSK
Your healthcare provider will look at the images from your cystogram to see if urine is leaking from your bladder. Based on what they see, they will decide if the urinary catheter can be removed.
If you will go home with the urinary catheter in your bladder, your nurse will give you the resource About Your Urinary (Foley) Catheter: How To Clean and Care for It. Follow the instructions in this resource to care for the urinary catheter.
At home
You can go back to your usual activities right away.
Drink 8 or more (8-ounce) glasses of liquids the day of your cystogram and the day after. Avoid liquids with caffeine (such as coffee, tea, and cola). This will help to rinse out your bladder and prevent infection.
If your urinary catheter was removed before you went home:
- Urinate as soon as you feel the urge to go. Don’t hold your urine for long periods of time.
-
For 2 to 3 days after your cystogram, you may have:
- A burning feeling when you urinate.
- Sudden, strong urges to urinate.
- Some urinary incontinence (trouble controlling when you urinate).
These things should get better each day. Call your healthcare provider’s office if they’re not better after 3 days or if they get worse.
Call your healthcare provider if you have:
- Trouble urinating or can’t urinate.
- An urge to urinate but have little or no urine.
- A feeling like your bladder doesn’t empty completely when you urinate.
- A fever of 101 °F (38.3 °C) or higher.
- Shaking chills.
- A burning feeling when you urinate that lasts for more than 3 days.
- Pain in your lower back.