This information describes your Medtronic implanted infusion pump, including how it works, how it’s placed, and how it’s refilled.
About Your Pump
You will get your medication through a Medtronic pump. Your pump is a small, programmable device made of titanium metal. It’s round and about the size of a hockey puck. The pump has a few main parts (see Figure 1).
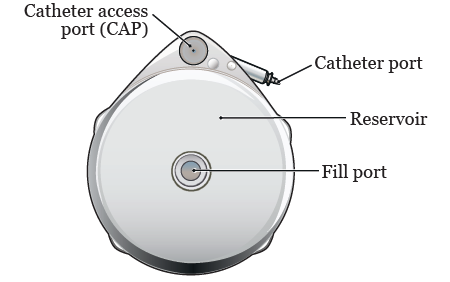
- The fill port is in the center of your pump. Medication is put into your pump through the fill port.
- The reservoir will hold your medication.
- The catheter is a small, flexible tube. It connects your pump to your hepatic artery (the main blood vessel that goes into your liver).
- The catheter access port (CAP) is used to send medications directly into your liver.
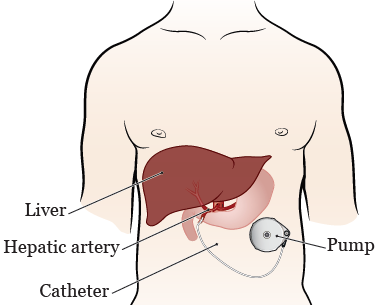
Your pump will be implanted (surgically placed) in your abdomen (belly) close to your liver. The medication will flow from your pump directly into your liver through the catheter that’s placed in your hepatic artery.
How Your Pump Is Implanted
You’ll have a surgery to implant your pump. Your nurse will give you more information and tell you how to get ready for your surgery.
You’ll be given general anesthesia (medication to make you sleep) before your surgery starts. Once you’re asleep, your doctor will make a small incision (surgical cut) in your lower abdomen. They’ll make a space between the skin and muscle and place your pump in this space. Then, they’ll place your pump’s catheter into your hepatic artery (see Figure 2).
While you’re in the operating room, your doctor will program your pump to deliver the medication to your liver at a constant rate. This is how you’ll receive medication regularly after your pump is placed.
Your surgery will take about 1½ to 2 hours. If you’re having other procedures done as well, it may take longer. After your surgery, you’ll stay in the hospital for 1 to 3 days, unless your doctor tells you otherwise.
Your doctor or nurse will give you an identification card that says you have an implanted device. You must carry this card at all times while you have your pump, both in the hospital and at home.
After your pump is placed, you may get stomach ulcers (sores in the lining of your stomach) from the catheter. This is because the catheter is close to your stomach and may irritate it. Your doctor will prescribe you medication to take at home to help keep this from happening.
About Your Flow Scan
Before you start using your pump, you’ll have an imaging procedure called a flow scan to make sure it’s working properly. The flow scan is usually done after your pump is implanted, while you’re staying in the hospital. Sometimes it’s done after you’re discharged from the hospital. Your healthcare provider will tell you when you’ll have the flow scan procedure.
During the flow scan, you’ll get injections of radioactive isotopes (radioactive liquids).
You’ll get the first injection of the radioactive isotope through an IV (intravenous) line in your arm or hand. After this injection, your nurse will use a special camera, called a gamma camera, to take pictures of your liver. This step will show the outline of your liver.
You’ll get the second injection of the radioactive isotope into your pump through the CAP. You may feel some pain from the prick of the needle while it’s put into the CAP. Getting the needle into the CAP can take up to 30 minutes.
Once the needle is in, your nurse will inject you with the radioactive isotopes and then a special liquid to flush the catheter. This will show how the isotope moves through the pump catheter into your liver to make sure it’s working. Then, your nurse will take more pictures of your liver and pump with the special camera. When your nurse has enough pictures, they’ll take the needle out of your catheter access port.
After the needle is taken out, you’ll need to lie still for 30 minutes while your nurse takes more pictures. If you think you’ll be uncomfortable lying in one position for a long time, talk with your doctor before your appointment.
The flow scan will take about 2 hours.
Before you go home, your nurse will fill your pump with medication. Your nurse will give you information about your medication and its possible side effects.
Activity Guidelines While You Have Your Pump
Recovery from the pump placement surgery usually takes about 4 weeks. After you recover, you can go back to doing most of your usual activities. But, there are some activities you should avoid. Follow the guidelines below on which activities to avoid. Talk with your healthcare provider if you have any questions.
Activities to avoid
- Avoid rough physical activities (such as contact sports). They can cause an injury to your pump site.
- Avoid strenuous exercise (such as running or jogging). It can make the catheter move out of place.
- Avoid lifting objects 10 pounds (4.5 kilograms) or heavier. This can make your pump move out of place.
- Avoid deep sea or scuba diving. You can swim or snorkel.
-
Avoid activities that raise your body temperature. They can make your medication flow faster. Do not:
- Place heating pads, electric blankets, or hot water bottles directly on your pump site.
- Go in a sauna or hot tub.
Magnetic resonance imaging (MRI)
It’s okay to have a magnetic resonance imaging (MRI) scan while you have a Medtronic implanted pump.
Refilling Your Pump
Follow your doctor’s instructions for how often you should refill your pump. If you’re receiving floxuridine (FUDR), you’ll have to refill your pump every 14 days (2 weeks). Your pump only holds enough medication for a limited amount of time.
It’s very important to go to all of your refill appointments. Your pump can run dry if it isn’t refilled regularly. If your pump runs dry and becomes damaged, you may not be able to keep using it for your treatment.
You might hear an alarm if your pump runs dry or stops working properly. You can read the “Understanding Pump Alarms” section of this site to hear what the alarms may sound like: www.medtronic.com/us-en/patients/treatments-therapies/drug-pump-cancer-pain/living-with/daily-living.html.
Call your healthcare provider if you:
- Can’t go to a refill appointment.
- Will be out of town at any point while you have your pump.
- Hear an alarm coming from your pump. You may need your pump checked.
How your pump is refilled
The procedure to refill your pump will take 15 to 20 minutes.
First, your nurse will clean your skin over your pump. They’ll put a needle that’s attached to a thin tube through your skin, into the fill port. The prick of the needle might be uncomfortable.
Your nurse will use a collection syringe to take out any medication in your pump from the last infusion and measure it.
Once your pump is empty, your nurse will put a syringe into the fill port to refill your pump with new medication (see Figure 3). You won’t have any discomfort while the medication is being refilled.
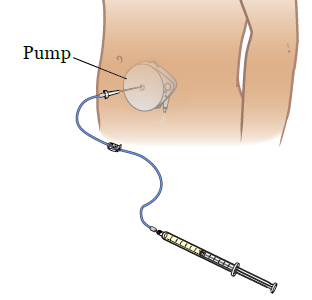
Once your pump is refilled with medication, your nurse will use the handheld programmer to reset your pump. Then it will start to deliver medication on a regular schedule again.
When to Call Your Healthcare Provider
Call your healthcare provider if you:
- Have a fever of 100.4 °F (38 °C) or higher.
- Have any signs of infection at your pump site, such as tenderness, drainage, or redness.
- Have swelling over your pump site.
- Can’t go to a scheduled refill appointment. Your pump may not work properly if you miss an appointment.
- Hear any alarms coming from your pump.
- Can’t go to a scheduled refill appointment.
- Have any questions or concerns.
