This information will help you get ready for your Pluvicto treatment at MSK. Pluvicto is a type of radionuclide (RAY-dee-oh-NOO-klide) therapy called radioligand therapy (RLT).
About Pluvicto
Pluvicto is a targeted radioactive therapy. It is used to treat PSMA positive metastatic castration resistant prostate cancer (mCRPC). This type of cancer is also called prostate cancer that has progressed.
Pluvicto has 2 main parts:
- The targeted part finds cancer cells and binds to them. It uses prostate-specific membrane antigen (PSMA) receptors on your cells.
- The radioactive part uses radiation (waves of energy) to harm and kill cancer cells.
Your healthcare provider will recommend Pluvicto treatment if your prostate cancer:
- Does not respond to hormone treatment that lowers your testosterone.
- Has spread to other parts of your body.
- Is found on a PSMA PET-CT scan or Pylarify® PET-CT scan.
You’ll get Pluvicto as an intravenous (IV) infusion. This is when medicine is put into your bloodstream through a vein over time.
Getting ready for your treatment
Before you get Pluvicto, you’ll need to have blood tests. Then you’ll meet with a healthcare provider from the Molecular Imaging and Therapy Service (MITS). MITS is sometimes called the Nuclear Medicine service. You can meet with them in-person at MSK’s main hospital or have a telemedicine visit.
During your appointment, your MITS provider will review your medical history and recent blood tests. They’ll use these to decide when to start your Pluvicto treatment. They will also review any recent scans you had.
Your MITS provider will also ask you about your medicines. Tell them every medicine you’re taking. This includes patches, creams, prescription medicine, and over-the-counter (not prescription) medicine.
Your MITS provider will decide it’s safe for you to start treatment. If it is, they’ll review the side effects with you. They’ll also give you information about your Pluvicto treatment schedule and talk about your treatment goals.
Pluvicto treatment schedule
Figure 1 below shows your Pluvicto treatment schedule.
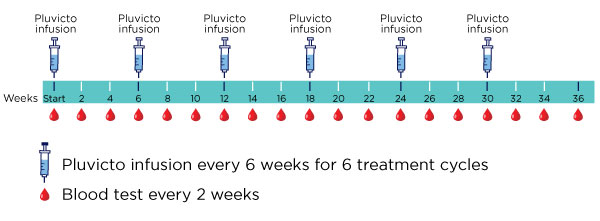
You’ll get Pluvicto as 6 separate infusions. The infusions are about 6 weeks apart. You will come to the main hospital at MSK for each infusion.
You will have regular blood tests to monitor your health. These tests will check:
- Your blood cell counts.
- Your nutrition.
- Your electrolyte levels.
- If your liver and kidneys are working normally.
You can have these blood tests done at the MSK location closest to you. Bring your appointment calendar with you to each treatment to schedule your next cycle and future lab appointments.
About your Pluvicto infusion visits
Your infusion visits will take most of the afternoon. Please do not schedule other appointments on your treatment days.
You should plan to be at your appointment for 3 to 4 hours. You can find the exact time in your MyChart account. You may want to bring a book or other things to keep yourself busy during your appointment. You can also bring food and a drink.
Where to go
Schwartz Cancer Research Building
1250 First Avenue (between East 67th and 68th Streets)
New York, NY 10065
Your Pluvicto infusion visits will be in the MITS therapy suite. To get to the suite:
- Enter the hospital through the entrance at 1250 First Avenue.
- Turn left at the security desk in the lobby. If you have questions or need an elevator instead of the stairs, ask the security guard for help.
- Go up the stairs and check in at the reception desk at the top of the stairs. You can wait in the waiting area.
What to expect when you arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having treatment on the same day.
When it’s time for your appointment, a staff member will bring you to the MITS therapy suite. You’ll sit in a private room with a TV and Wi-Fi.
Before your infusion, your MITS provider will review your:
- Medical history
- New or recent symptoms
- Medicines
- Blood counts
They will also do a physical exam and answer any questions you have.
A nurse will measure your vital signs, including your pulse, temperature, breathing, and blood pressure. They will also place an IV line (thin, flexible tube) into a vein in each of your arms.
Some people have a central venous catheter (CVC). This can be one of the following:
- An implanted port (Mediport®).
- A tunneled chest catheter.
- A peripherally inserted central catheter (PICC).
If you have a CVC, the nurse will place an IV line into it. They will place the other IV line into a vein in your arm or hand.
If you do not have a CVC, they will place an IV line into each of your arms or hands.
Medicine you’ll get
You’ll get a few different medicines during your infusion visits.
First, you’ll get anti-nausea medicine. This is medicine to keep you from vomiting (throwing up) or feeling nauseous (like you’re going to throw up).
After the anti-nausea medicine, your nurse will connect a saline hydration to one of your IV lines. Saline hydration is water with a small amount of salt. You’ll get this infused (put into your bloodstream) slowly, over 2 hours.
Your MITS provider will connect Pluvicto medicine to your other IV line. Your Pluvicto infusion will take about 20 minutes.
If you have friends or family with you, they cannot be in the room during your Pluvicto infusion. A staff member will ask them to wait in the waiting area to avoid being exposed to radiation.
Side effects
During and after your Pluvicto infusion, you may have the following side effects:
- Fatigue (feeling more tired and weak than usual).
- Dry mouth.
- Nausea.
- Decreased appetite.
- Change in bowel movements (poop). This can be constipation (pooping less often than usual) or diarrhea (loose or watery poop).
- Low blood counts. A low blood count may delay the start of your treatment.
A nurse will stay with you during your entire treatment to help with these symptoms if they happen.
Nuclear medicine scan
After the saline hydration, you’ll have a nuclear medicine scan. This is done to check where the Pluvicto went in your body. You will lie down during the scan.
The scan will take about 10 minutes. You can leave the hospital after the scan.
Your Pluvicto infusion visit and scan will take a total of 3 to 4 hours.
Radiation safety measures
After your Pluvicto infusion, there will be radiation coming from your body. A radiation safety staff member will talk with you about your radiation safety measures before you leave your injection appointment. They will also give you written instructions to follow at home.
To keep from exposing others to radiation, follow the radiation safety instructions below. You must follow these safety measures for 2 to 11 days. This will depend on your specific Pluvicto treatment.
- Avoid being in close physical contact with other people for a long period of time. You should stay at least 3 feet (about an arm’s length) away from other people most of the time. It’s OK to hug or be in close contact with another person for a short period of time.
- Do not use public transportation, such as a bus or train, right after your infusion appointment. If you do need to take public transportation soon after treatment, contact radiation safety for more details. It’s OK to use a car service.
- If you’re driving with another person in the car, sit as far away from them as you can. You should also do this if you’re using a car service.
- Practice good hygiene, such as washing your hands well with soap and water after using the bathroom. The radioactive material will leave your body through your body fluids during the first few weeks after treatment. This includes blood, urine (pee), saliva.
In general, you must:
- Stay at least 3 feet away from others for the first few days after treatment.
- Sleep alone for 4 days.
- Avoid holding or sleeping next to small children or pregnant people for 9 to 11 days.
Some security equipment, such as at the airport or outside a tunnel, can detect very small amounts of radiation. You will get a card that says you got radioactive medicine. It says you can give off small amounts of radioactivity for up to 2 months after your treatment. Show this card to law enforcement if they stop you at a checkpoint.
If you have any questions about radiation safety, call 212-639-7391 Monday through Friday from to
After your Pluvicto infusion visits
There may still be traces of radiation in your body a month after a Pluvicto infusion. Follow the radiation safety instructions. It’s very important to follow these instructions in the bathroom to clean or flush bodily fluids, such as urine.
Drink lots of liquids after each infusion. This will help the radiation leave your body more quickly.
Some people may need medical care during the first 2 weeks after a Pluvicto infusion. This includes an operation or a stay in the hospital. If you do, tell one of your healthcare providers that you were treated with radioactive Lutetium-177. There can still be some radiation in your body.
Tell a medical provider or staff member that you’ve been treated with radioactive Lutetium -177 if:
- You need to give blood, urine, or stool (poop) samples during the first 10 days after a Pluvicto infusion. The samples you give might have radiation in them.
- If you need medical care during the first month after a Pluvicto injection. This includes needing an operation or hospital stay.
The medical provider or staff member should take universal precautions. They do not need to take any extra safety measures.
When to call your care team
Watch the insertion sites for 48 hours (2 days) after your infusion. Your infusion sites are where the IV lines went into your body.
Call your care team if you notice any changes in the area, such as:
- Pain or a burning feeling.
- Redness or other changes to your skin color.
- Swelling.
- Broken skin.
- Blisters or liquid draining.
- Numbness, tingling, or other changes in sensation (feeling).
- Warm or hot skin.
Tell your healthcare provider right away if you have any new symptoms or if your symptoms get worse. This includes urinating (peeing) less often or urinating much smaller amounts than usual.
Contact information
If you have any questions or concerns, please call the Molecular Imaging and Therapy Service.
- Monday through Friday from 9 a.m. to 5 p.m., call 212-639-3146. Ask for the Molecular Imaging and Therapy Service nurse.
- After 5 p.m., during the weekend, and on holidays, call 212-639-2000. Ask for the Molecular Imaging and Therapy Service fellow on call.