This information will help you learn about your urostomy and urostomy pouching (bag) system.
About your urostomy
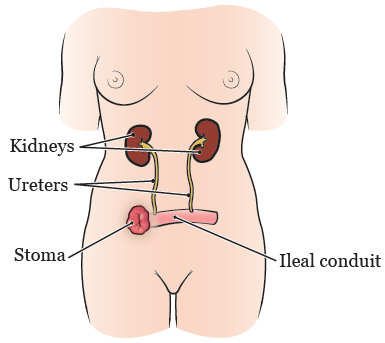
A urostomy (yoo-ROS-toh-mee) is surgery to make an opening, called a stoma, in your abdomen (belly). This opening will be where urine leaves your body. The type of urostomy you had was an ileal conduit (IH-LEE-ul KON-doo-it).
Your doctor used a small piece of your intestine called the ileum (IH-lee-um) to make the ileal conduit. One end of the ileum was attached to your ureters. The other end was attached to the stoma.
After surgery, your urine (pee) flows from your kidneys, through your ureters and ileal conduit, and out of your stoma (see Figure 1). You will wear a urostomy pouching (bag) system over your stoma to catch and hold the urine. A urostomy pouching system is sometimes called a urostomy appliance.
Your stoma should be a deep pink or red color all the time. If your stoma looks grey, brown, or black, contact your doctor right away.
You will not be able to control the flow of urine from your stoma. The urostomy pouching system over your stoma will catch and hold the urine.
There are a few types of urostomy stomas. Your wound, ostomy, and continence (WOC) nurse will tell you which type you have and answer your questions.
About your urostomy pouching (bag) system
A urostomy pouching (bag) system has 2 parts. A wafer is the part that sticks to your skin. The pouch is the bag that holds your urine.
With a 2-piece pouching system, the wafer and the pouch are separate pieces that can be taken apart. With a 1-piece pouching system, the wafer and pouch are connected.
You will use different types of pouching systems in the hospital and at home. This is because your stoma will get smaller as it heals. It often takes about 6 to 8 weeks for your stoma to get to its permanent size.
In the hospital
While you’re in the hospital, you will learn how to care for your urostomy stoma and pouching system.
Most people use a 2-piece pouching system while they’re in the hospital.
At home
After you’re discharged (released) from the hospital, you will use either a 2-piece or a 1-piece pouching system. A home care nurse will visit you to help you learn how to care for your stoma and pouching system.
You may use different pouching systems as your body heals and your stoma gets smaller. You will have appointments with an outpatient WOC nurse from MSK.
They will look at your stoma with you. They will keep track of how your stoma is healing. They will help you choose the pouching system and ostomy accessory products that are best for your body. Ostomy accessory products are products you can use along with your pouching system.
Follow-up appointments
Your WOC nurse may not be available when you contact your doctor’s office. They will get your message and contact you.
Your first appointment with your outpatient WOC nurse will be 2 weeks after you’re discharged from the hospital. It’s also helpful to schedule follow-up appointments with them 2 to 3 months and 6 months after your surgery.
You should also contact your WOC nurse if you have skin issues or questions about your pouching system.
You may lose some weight when you’re first recovering after surgery. Over the 3 to 6 months after surgery, you will probably gain back some of this weight.
During this time, you may notice some small changes in the shape of your abdomen. These changes can cause your pouching system to fit differently and be uncomfortable. If this happens, contact your WOC nurse. They can recommend a pouching system that’s more flexible and moves with your body.
You may also want to choose a more flexible pouching system if it’s uncomfortable when you bend, twist, or work out. Your WOC nurse will help you find a system that works best with your body and activities.
Contact your doctor’s office if you have questions or concerns, or to make an appointment with your WOC nurse.
Positioning your pouching system
Position your pouch so it points down and can be tucked into your pants or underwear. You can also fold it, if you want to. You can also try special underwear or concealment bands. You can find them online at www.ostomysecrets.com or www.stealthbelt.com, among other places.
Wearing a belt or suspenders
You can wear a belt or suspenders on your pants when you’re wearing your pouching system. If you choose to wear a belt, wear it above or below your stoma. The belt can cause irritation, bleeding, or an overgrowth of tissue if it’s right on your stoma.
Preparing an emergency kit
Prepare a small emergency kit with a pre-cut wafer, a pouch, and a few gauze pads. Always keep the emergency kit with you so you can change your pouch if it leaks.
Keep your emergency kit out of direct sunlight or heat.
Ordering supplies
Ostomy supply companies
There are 2 main types of ostomy supply companies.
- Ostomy supply distributors are companies that sell ostomy products. They sell supplies made by many companies. You will order your urostomy supplies from an ostomy supply distributor.
- Ostomy supply manufacturers are companies that make ostomy products. You can call an ostomy supply manufacturer for information about their products. You also can ask for a sample of their products. You cannot buy products right from the manufacturer.
When to order supplies
Order more supplies when you have only 1 box of pouches or wafers left. You can order from one of these ostomy supply distributors:
|
|
Choose an ostomy supply distributor that accepts your health insurance. You can find out by calling the distributor.
Ostomy accessory products
There are many kinds of ostomy accessory products. Examples of ostomy accessory products are:
- Barrier ring or protective seal: This goes around the base of your stoma and helps the wafer fit better. It can help keep urine from leaking under the wafer.
- Elastic barrier strips: These go over the wafer and help keep it from coming off your skin. They also help to waterproof the wafer.
- Ostomy belt: This attaches to the wafer and wraps around your waist. It helps to secure the pouching system.
- Stoma guard: This goes over your stoma and pouching system to provide extra protection. It can be helpful if you play contact sports.
You probably will not need to use all these accessory products. Your WOC nurse will give you more information about the accessory products that may help you the most.
Night drainage system
A night drainage system is a bag or bottle that connects to the bottom of your pouch. It holds more urine than your normal pouch.
It’s important to use a night drainage system when you sleep to keep your pouch from getting too full. If it’s too full, it can leak, or urine can flow back into your stoma and cause an infection. Using a night drainage system can also help you avoid having to get up at night to empty your pouch.
You will need to use an adaptor to connect the night drainage system to your pouch. The adaptor is included in your box of pouches.
Caring for your night drainage system
Each morning, empty the urine from the night drainage bag or bottle into the toilet.
You can make a solution of 1 part white vinegar and 3 parts water. Fill the bag or bottle with the solution. Let it soak for 2 to 4 hours. After you soak it, pour out the solution and let the bag or bottle air dry.
Use a special cleanser, such as the Hollister M9™ Crystallizer cleansing system, if:
- The bag or bottle has a very strong odor (smell).
- You’re at high risk for infection.
You can buy these cleansers online or through an ostomy supply distributor.
Replace your night drainage system every 2 weeks.
You may have problems with your night drainage system tubing coming loose. If so, you can tape the connections between the night drainage system and your pouch. If you move around a lot while you sleep, use a leg stabilizer or Foley® catheter holder. You can order these accessories when you order your supplies and extension tubing, if needed.
Leg drainage bag
A leg drainage bag is a pouch that holds more urine than your normal pouch. You may want to use a leg drainage bag if you’re traveling. You can use it if you cannot get to a toilet to empty your pouch, such as if you’re in traffic.
Your health insurance plan may not pay for leg drainage bags. You can call the ostomy supply distributor to find out if leg drainage bags are covered by your insurance. If not, you can buy them from a surgical supply store.
Caring for your leg drainage bag
When the pouch is getting full, empty the urine from the leg drainage bag into the toilet. Wash it after you empty the bag. You can use warm water, or a mixture of ¼ cup white vinegar and 1 cup water. After you wash the drainage bag, let it air dry.
Use a special cleanser, such as the Hollister M9™ Crystallizer cleansing system, if:
- The bag has a very strong odor (smell).
- You’re at high risk for infection.
You can buy these cleansers online or through an ostomy supply distributor.
Replace your leg drainage bag every week, no matter how many times you use it.
Finding out about new products
You can find out about new products by:
- Asking your WOC nurse.
- Calling ostomy supply manufacturers to ask for samples of their latest products.
- Searching for urostomy products online.
- Joining an online chat room or local support group for people with urostomies. Often, other people dealing with the same issues know of products that can meet your needs.
Make sure you’re looking at urostomy products, not fecal pouches. Read the “Resources” section for a list of online support groups and websites to help you find local support groups. Make sure you talk with your WOC nurse before trying any new urostomy products.
Changing your urostomy pouching (bag) system
You should change your pouching (bag) system about every 3 to 4 days. If it’s leaking urine, change it right away. It’s best to change your pouching system in the morning before you drink any liquids. There’s often less urine coming out of your stoma in the morning.
The first time you change your pouching system, you will be sitting in your hospital bed. As you heal, you can start changing your pouching system wherever you’re most comfortable.
Most people like to stand in the bathroom in front of the mirror. You can also remove your pouching system and clean around your stoma as part of your normal shower routine.
To learn more about changing your pouching system, read Changing Your Urostomy Pouching (Bag) System at Home.
What to do if you see blood on your stoma
Your stoma has many blood vessels and can bleed easily. It’s normal to see a small amount of blood on the gauze or tissue when you’re cleaning your stoma. The bleeding should stop on its own within a few minutes. If you take a blood thinner or aspirin, you may bleed more easily and for a longer time. Apply pressure to your stoma to help stop the bleeding.
Call your doctor if the bleeding does not stop after 10 to 15 minutes. You may need to go to MSK’s Urgent Care Center or your local emergency room. Your doctor will tell you what to do.
Call your doctor right away if there’s blood in your urine or coming from the inside of your stoma.
About wearing gloves
You can decide if you want to wear gloves when you change your pouching system. Before your surgery, you did not wear gloves when urinating (peeing). You do not need to wear them now. However, you may prefer to wear gloves when you change your pouch because some urine could get on your fingers.
Showering with your stoma
It’s very important to shower every day. This will help keep your skin clean.
Your pouching (bag) system is waterproof. Keep your pouching system on while you shower.
On the days you’re changing your pouching system, you can take your pouching system off and shower without it, if you want. Urine will keep flowing from your stoma while you shower.
Shower the same way you did before your surgery. Do not use perfumed or oil-based soaps around your stoma.
Problems caused by your urostomy
Contact your doctor’s office if you have any of the problems below. They will share your message with your WOC nurse, and your WOC nurse will reach out to you.
Skin problems
If the leakage does not stop after you change your wafer, contact your WOC nurse. You may need another system that fits better to avoid leakage.
Tell your WOC nurse if you have any problems with the skin around your stoma (peristomal skin). Most common skin problems happen if urine gets under the wafer or if you have allergies to your ostomy products.
The Wound, Ostomy, and Continence Nurses Society has a tool to help you figure out if you have any peristomal skin problems. You can find it at http://psag-consumer.wocn.org
Tissue buildup
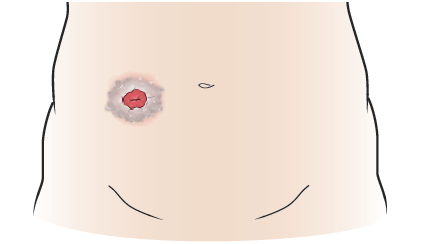
One common skin problem is a buildup of tissue on the skin around your stoma. The tissue may look greyish, purplish, wart-like, or have white spots (see Figure 2). It can cause pain around your stoma. The buildup is caused when your skin is exposed to urine all the time. If you have tissue buildup, call your doctor’s office to make an appointment with your WOC nurse.
If you’re having problems with tissue buildup around your stoma, you may need to:
- Cut or mold your wafer or get a different pre-cut wafer.
- Use a different type of wafer.
- Apply a barrier ring or protective seal to your wafer. Examples are a Colly-Seel™ disc, Coloplast Brava® Protective Seal, or Hollister slim CeraRing.
You may also need to treat the skin right around your stoma each time you change your pouching (bag) system. To do this:
- Mix ¼ cup of white vinegar with ¾ cup of water.
- Soak a gauze pad in the mixture. Place the gauze pad on your skin for 20 minutes.
- Rinse your skin with water.
- Dry your skin well and apply a new wafer.
Allergic reaction
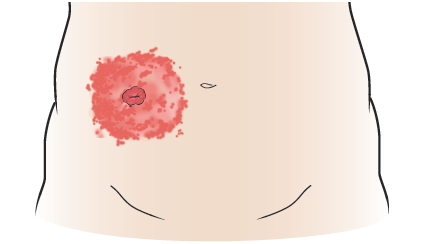
Another common skin problem is an allergic reaction to one of your ostomy products. You may have redness or welts on the skin around your stoma (see Figure 3). You may also have itching, burning, or discomfort. If you think you’re having an allergic reaction, call your doctor’s office. You may need to see a dermatologist (skin doctor).
If you’re having an allergic reaction, you will need to try another brand of wafer and pouch.
Rash
If you get a rash, tell your doctor or WOC nurse. They will give you suggestions for how to treat it.
Urinary tract infections (UTIs)
The signs and symptoms of a UTI are:
- Urine that smells worse than usual
- Cloudy urine
- Back pain
- Nausea (feeling like you’re going to throw up) and vomiting (throwing up)
- Loss of appetite
- Fever of 100.4 °F (38 °C) or higher
If you think you have a UTI, call your doctor’s office.
To keep from getting a UTI:
- Drink 6 to 8 (8-ounce) cups of liquids every day. It’s best to drink water.
- Limit the amount of alcohol and caffeine you drink.
- Use a pouch that has an anti-reflux valve and use a night drainage system. This keeps urine from sitting on your stoma and causing an infection.
- Empty your pouch when it’s ⅓ to ½ full.
You can also ask your doctor if you can take vitamin C (about 500 to 1,000 milligrams) and a sugar-free cranberry pill daily. These will make your urine more acidic and may help prevent UTIs. It will help with your urine’s odor (smell), and keep your skin from being harmed.
Hernias
A hernia is when a loop of bowel (intestine) pokes through a weak area of muscle. This causes a bulge to form. Hernias often do not cause any symptoms. If you see a bulge around your stoma, contact your doctor or WOC nurse.
Tips to avoid getting a hernia
Often, the abdominal muscle around your stoma is weak. There are ways to try to keep from getting a hernia. Avoid constipation (straining to pass bowel movements), coughing a lot or very strongly, heavy lifting, or straining.
It takes up to a year for the inside of your body to heal after surgery. Pay attention to how your body feels. If you feel pain during any activities, stop doing them. Call your doctor’s office if the pain does not go away.
Treating a hernia
If you have a hernia, your WOC nurse can suggest a hernia support belt. These belts are made to fit your body. You can also use a girdle or biking shorts to support the hernia. If you use these, you must cut out a hole for your urostomy pouch.
Using a hernia support belt, girdle, or biking shorts will not cure the hernia or keep it from getting worse. But they can make you feel more comfortable and pull in the bulge to help your clothes fit better.
Hernias often are not treated unless they become blocked, twisted, or cause pain or other problems. Call your doctor right away if you have:
- Nausea
- Vomiting
- Pain in your abdomen
- Swelling in your abdomen
Traveling after a urostomy
You should not base your travel choices on the fact that you had a urostomy. Here are some tips to help you manage traveling with your pouching (bag) system:
- Bring extra supplies, just in case you have trouble getting them while you’re away.
- If you’re taking an airplane, train, or bus, carry your supplies with you. Do not put them in your checked luggage. This will help you be ready if you’re separated from your luggage.
- Avoid driving a car for 4 to 6 weeks after your surgery, unless your doctor tells you otherwise. You may wear a seat belt loosely or place a small pillow over your stoma and under your seat belt. You can also use an ostomy seat belt protector. Check with your ostomy supply distributor or ask your WOC nurse for more information.
- Talk with your WOC nurse about travel options. You may want to use a leg drainage bag if it’s hard to get to a toilet to empty your bag.
- If you’re traveling by airplane, you may want to get a Travel Communication Card from the United Ostomy Associations of America (UOAA). To learn more, call 800-826-0826 or visit www.ostomy.org/traveling-with-an-ostomy.
Getting ready for medical visits
Always bring extra urostomy supplies with you. Many pharmacies and medical centers do not have urostomy supplies. You may need an extra set.
Imaging scan with contrast
If you’re having a scan with contrast, bring an extra set of urostomy supplies. Also bring a leg drainage bag or night drainage system.
For the scan, you will need to drink more liquids than usual. This will help the contrast leave your body. But drinking more also means your body makes more urine. You may need to change your pouching (bag) system if you leak because you’re making more urine than usual.
If you live 1 hour or more away from the hospital, empty your bag before leaving. You may also need to empty it on the trip home or use a leg drainage bag. You may also want to keep a portable urinal or other container in your car in case of an emergency.
Chemotherapy or immunotherapy
If you’re having chemotherapy or immunotherapy, bring an extra set of urostomy supplies. Chemotherapy or immunotherapy can cause your body to make more urine. It can also make your skin more sensitive or change the way the wafer sticks to your skin. You may need to change your wafer more often during chemotherapy or immunotherapy. This protects your skin and prevents leakage.
Other procedures
You may have a procedure where your care team needs to access your stoma. If so, you may need to switch to another type of pouching system. For example, you may need to switch from a 1-piece system to a 2-piece system. Your doctor or nurse will talk with you before the procedure.
If you have any problems, contact your WOC nurse.
Resources
MSK support groups
Bladder cancer support group
This is an online support and education group. It’s for people who have bladder cancer or who have been treated for bladder cancer. People share their personal experiences and offer practical and emotional support for one another. It’s led by an MSK social worker, nurse, and WOC nurse.
This group meets the second Thursday of each month from noon (12 p.m.) to For more information or to register, contact your MSK social worker. You can also send a message to your care team through MSK’s patient portal, MSK MyChart. They can connect you with an MSK social worker. A member of your care team will review your message and respond within 2 business days (Monday through Friday).
Resources for finding WOC nurses
Wound, Ostomy, and Continence Nurses Society
www.wocn.org/learning-center/patient-resources
Visit this website to find a WOC nurse in your area.
You can also call your ostomy supply manufacturer or distributor to ask for information about WOC nurses in your area. Many WOC nurses can only see you if there’s an outpatient clinic at their hospital. Or, they can only see you if you have a doctor at their hospital.
Resources for finding urostomy support groups
Bladder Cancer Advocacy Network (BCAN)
www.bcan.org
Visit this website for information about bladder cancer. To join an online support group sponsored by the BCAN, visit www.inspire.com/groups/bladder-cancer-advocacy-network.
Inspire
www.inspire.com
Visit this website to find online ostomy support groups.
United Ostomy Associations of America, Inc. (UOAA)
www.ostomy.org
Visit this website to find an ostomy support group, including both online support groups and groups in your area. You can also find tips for traveling with an ostomy and download the UOAA’s Travel Communication Card.
Resources for managing skin irritation around your stoma
Peristomal Skin Assessment Guide
http://psag-consumer.wocn.org
Visit this website if the skin around your stoma is irritated. On the website, you will answer questions to find out more about the type of skin irritation you have. It will tell you what you can do to manage it.
Remember to always contact your WOC nurse if you think the skin around your stoma is irritated.
Resources for ostomy supplies
Manufacturers: Contact the ostomy supply manufacturer that makes your pouching (bag) system. Every ostomy supply manufacturer has a program to help you with their supplies. Some manufacturers also have WOC nurses that can help you.
Distributors: Some ostomy supply distributors also have a WOC nurse who can help you. Call your distributor for more information.
Resources for ostomy concealment garments
Ostomy concealment garments are clothes to help hide your pouching system.
C&M Ostomy Supplies
www.cmostomysupply.com
Visit this website to buy ostomy garments, including pouch covers and stoma guards.
Nu-Hope
www.nu-hope.com
Visit this website to buy a custom hernia support belt made to fit your body.
Ostomysecrets
www.ostomysecrets.com
Visit this website to buy ostomy garments.
Safe n’ Simple
https://sns-medical.com/products/support-belts
Visit this website to buy a hernia support belt.
Stealth Belt
www.stealthbelt.com
Visit this website to buy ostomy garments.
