This information will help you get ready for your Bravo capsule test at MSK.
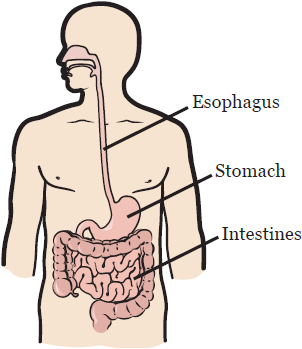
The 48-hour (2-day) Bravo capsule test checks the amount of acid that comes back into your esophagus from your stomach. When this happens, it is called acid reflux. Your esophagus is the tube that carries food and liquids from your mouth to your stomach (see Figure 1).
Your Bravo capsule test can tell your healthcare provider how much acid reflux you have. It can also tell the length of time you experience it. Your care team will get this information as you go about your usual activities. This procedure is also used to determine if you have gastroesophageal reflux disease (GERD).
You will have your Bravo capsule test during an upper endoscopy procedure. Your healthcare provider will use a flexible tube called an endoscope to see the inside of your esophagus on a video monitor. A small capsule will be placed temporarily on the wall of your esophagus. The capsule will measure the amount of acid reflux you have. This information will then be sent to a receiver you will wear on your waistband or belt.
Before your procedure
Ask about your medicines
You may need to stop taking some of your medicines before your procedure. Talk with your healthcare provider about which medicines you should stop taking. Some common examples are:
- Proton pump inhibitors, such as rabeprazole (Aciphex®), omeprazole (Prilosec®), lansoprazole (Prevacid®), pantoprazole (Protonix®), and esomeprazole (Nexium®).
- Histamine type 2 blockers (H2 blockers), such as nizatidine (Axid®), famotidine (Pepcid®), cimetidine (Tagamet®), and ranitidine (Zantac®).
Medicines for diabetes
If you take insulin or other medicines for diabetes, ask the healthcare provider who prescribes your medicine what you should do the morning of your procedure. You may need to change the dose before your procedure.
Get a letter from your healthcare provider, if needed
If you have an automated implanted cardioverter-defibrillator (AICD), you will need to get a clearance letter from your cardiologist (heart doctor) before your procedure.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
3 days before your procedure
Talk with your endoscopy nurse
Your endoscopy nurse will call you 3 days before your procedure. They will review the instructions in this resource with you and ask you questions about your medical history. Your nurse will also review your medicines and tell you which to take the morning of your procedure.
The day before your procedure
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-7606.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
If you need to cancel your procedure, call the GI scheduling office at 212-639-5020.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
The day of your procedure
Things to remember
- Take only the medicines you were instructed to take the morning of your procedure. Take them with a few sips of water.
- Take off all jewelry, including body piercings. The equipment used during your procedure can cause burns if it touches metal.
- Do not put on any lotion, cream, deodorant, makeup, powder, cologne, or perfume.
- Leave all valuables, such as credit cards, jewelry, and your checkbook, at home.
- If you wear contacts, wear your glasses instead.
What to bring
- A list of all the medicines you take at home, including the dose.
- Your rescue inhaler (such as albuterol for asthma), if you have one.
- A case for your glasses.
- Your Health Care Proxy form, if you have filled one out.
Where to go
Your procedure will take place at one of these locations:
-
David H. Koch Center
530 East 74th Street
New York, NY 10021
Take the elevator to the 8th floor. -
Endoscopy Suite at Memorial Hospital (MSK’s main hospital)
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
Take the B elevator to the 2nd floor. Turn right and enter the Endoscopy/Surgical Day Hospital Suite through the glass doors.
Visit www.msk.org/parking for parking information and directions to all MSK locations.
What to expect
Once you arrive at the hospital, doctors, nurses, and other staff members will ask you to state and spell your name and date of birth many times. This is for your safety. People with the same or similar names may be having procedures on the same day.
After changing into a hospital gown, you will meet your nurse. They will place an intravenous (IV) catheter into a vein, usually in your hand or arm. At first, you will get fluids through the IV, but it will be used later to give you anesthesia (medicine to make you sleepy). Your nurse will also check your heart rate, breathing, and blood pressure.
Your healthcare provider will explain the procedure, and answer any questions you have. They will also ask you to sign a consent form stating that you agree to the procedure.
When it’s time for your procedure, you will be taken to the procedure room and helped onto an exam table. You will get anesthesia through your IV, which will make you fall asleep. You will have sensors (electrodes) attached to your skin, nose, and arm to monitor your heart, breathing, and blood pressure. You will also get oxygen through your nose. Once you’re asleep, your healthcare provider will place the capsule into your esophagus.
After your procedure
In the recovery room
You will wake up in the recovery room. Your nurse will continue to monitor your heart rate, breathing, and blood pressure. Once you’re fully awake, your nurse will take out your IV.
You will get a receiver to wear on your waistband or belt. This receiver shows how much acid reflux you have, which is measured by the capsule placed in your esophagus. You will also get a diary to fill out for 2 days. Your nurse will explain your discharge instructions to you and your caregiver before you go home.
At home
For 48 hours (2 days) after your procedure, make sure you record the following in your diary:
- All the symptoms you have, such as coughing, heartburn, and burping food into your mouth.
- All the medicines you take.
- Everything you eat and drink.
- The time you eat and drink.
- When you lie down.
It’s important that you eat, drink, work, and exercise as you normally would. Avoid the following because they will affect your test results:
- Foods high in acid, such as coffee, orange juice, cranberry juice, and soda.
- Gum and throat lozenges.
- Snacking between meals.
Keep the receiver on your waistband or belt at all times. When you shower, keep the receiver within 3 feet (about 1 meter) of your body in the bathroom. If it’s too far away, it will beep. Do not let the receiver get wet.
You may have some discomfort in your chest after your procedure. You can take acetaminophen (Tylenol®) to relieve this discomfort.
The capsule will pass through your system and come out during a bowel movement, but you might not see it.
Do not have magnetic resonance imaging (MRI) for 30 days after your capsule is placed.
Follow-up
You must return the receiver and your diary to your healthcare provider during your follow-up appointment. Your visit will be 48 hours after your procedure.
When to call your healthcare provider
Call your healthcare provider if you have:
- A fever of 101 °F (38.3 °C) or higher.
- Severe or constant stomach pain, hardness, or bloating.
- Severe or constant pain in your chest.
- Trouble swallowing.
- Nausea (feeling like you’re going to throw up) or vomiting (throwing up).
- Severe or constant bleeding from your nose.
- Any unexplained or unexpected problems.