This information will help you understand what lymphedema is and your risk for developing it.
About Your Lymphatic System
Your lymphatic system has 2 jobs:
- It helps fight infection.
- It helps drain fluid from areas of your body.
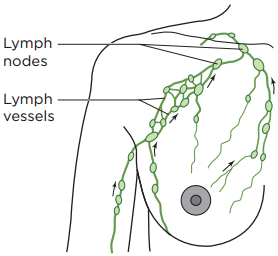
Your lymphatic system is made up of lymph nodes, lymphatic vessels, and lymphatic fluid (see Figure 1).
- Lymph nodes are small bean-shaped glands located along your lymphatic vessels. Your lymph nodes filter your lymphatic fluid, taking out bacteria, viruses, cancer cells, and other waste products.
- Lymphatic vessels are tiny tubes, like your blood vessels, that carry fluid to and from your lymph nodes.
- Lymphatic fluid is the clear fluid that travels through your lymphatic system. It carries cells that help fight infections and other diseases.
During surgery for breast cancer, your doctor may remove some of your lymph nodes to see if the cancer has spread. The lymph nodes that may be removed are:
- Sentinel lymph node(s). These are the first node(s) in your axilla (armpit) that receive drainage from the breast tumor. This node(s) is identified by injecting a special dye into your breast.
- Axillary lymph nodes. These are a group of nodes in your axilla that drain the lymph fluid from your breast and arm. If any cancer cells are found in your sentinel node(s), additional axillary lymph nodes may be removed. The number of nodes varies from person to person.
Sometimes, removing lymph nodes can make it hard for your lymphatic system to drain properly. If this happens, lymphatic fluid can build up in the area where the lymph nodes were removed. This extra fluid causes swelling called lymphedema.
Lymphedema can develop in the arm, hand, breast, or torso on your affected side (the side where your lymph nodes were removed).
Understanding Your Risk of Developing Lymphedema
Most people don’t develop lymphedema after surgery, but some do. It’s hard to know a person’s risk of developing lymphedema because:
- There’s no standard test for diagnosing lymphedema.
- Removing or injuring lymph nodes affects people differently.
- Lymphedema can develop soon after surgery, or it can develop years later.
- Current cases of lymphedema can be caused by older treatment methods.
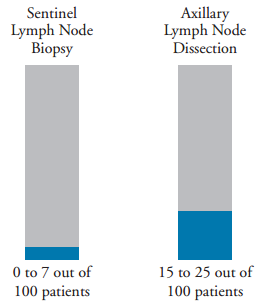
Your risk of developing lymphedema depends on how your lymph nodes are removed (see Figure 2). There are 2 types of surgeries used to remove lymph nodes: a sentinel lymph node biopsy and an axillary lymph node dissection.
During a sentinel lymph node biopsy, between 1 and a few lymph nodes are removed from your armpit and checked for cancer cells. The risk of developing lymphedema after a sentinel lymph node biopsy is low. About 0 to 7 out of every 100 people who have a sentinel lymph node biopsy develop lymphedema.
During an axillary lymph node dissection, more than a few lymph nodes are removed from your armpit. This is done to remove additional lymph nodes that may have cancer cells. The risk of developing lymphedema after an axillary lymph node dissection is higher than it is after a sentinel node biopsy. About 15 to 25 out of every 100 people who have an axillary lymph node dissection may develop lymphedema.
Damage to your lymphatic system can also increase your risk of developing lymphedema. The following things can damage your lymphatic system:
- Radiation therapy to your affected armpit
- An infection or severe injury (such as a serious burn) in your affected arm, hand, fingers, or breast after surgery
- Tumor growth in or near your armpit on your affected side
- Being overweight when you’re diagnosed with breast cancer
- Gaining or losing more than 10 pounds (4.5 kilograms) per month after your surgery
There’s no way to know for sure who will develop lymphedema.
Lowering Your Risk of Developing Lymphedema
Doing the following things may help lower your risk of developing lymphedema.
- Stay at or safely work towards a healthy body weight.
-
Exercise and stretch your muscles regularly. Talk with your doctor or nurse about which exercises are right for you.
- When you resume exercise and activity, build up slowly and gradually. If you feel discomfort, stop and take a break. Exercise shouldn’t cause pain.
-
If you get a cut or scratch on your affected arm or hand:
- Clean the area with soap and water.
- Apply antibacterial ointment, such as Bacitracin® or Neosporin®.
- Cover the area with a bandage, such as a Band-Aid®.
-
If you get a burn on your affected arm or hand:
- Apply a cold pack to the area or run the area under cool tap water for about 10 minutes.
- Clean the area with soap and water.
- Cover the area with a bandage, such as a Band-Aid.
- If you notice any signs of infection (such as redness, swelling, skin that’s warmer than usual, or tenderness), call your healthcare provider.
If you’re having a sentinel lymph node biopsy:
- It’s OK to use your affected arm for blood draws, injections (shots), intravenous (IV) lines, and blood pressure measurements. But, ask your healthcare providers to try to use your unaffected arm if it’s available.
- If you start to notice any signs of lymphedema, always use your unaffected arm. If this isn’t possible, talk with your healthcare provider about which arm is safest to use.
If you’re having an axillary lymph node dissection:
- Read the resource Hand and Arm Guidelines After Your Axillary Lymph Node Dissection for information about lowering your lymphedema risk after your procedure. Your healthcare provider will give you a copy, or you can read it online.
Signs of Lymphedema
Some mild swelling after surgery is normal. The swelling may last for up to 6 weeks. It’s often temporary and will gradually go away. You may also feel pain or other sensations, such as twinges and tingling, after surgery. These feelings are common and aren’t necessarily signs of lymphedema.
If you’re at risk of developing lymphedema, watch for these signs in your affected arm, hand, breast, and torso:
- A feeling of heaviness, aching, or pain
- A tight feeling in your skin
- Less flexibility
- Swelling
- Skin changes, such as tightness or pitting (skin that stays indented after pressing on it)
If you have any signs of lymphedema or aren’t sure, contact your healthcare provider.
