This information explains your intrathecal pump. It explains how it works, how it’s placed, and how it can help you manage your pain.
About your intrathecal pump
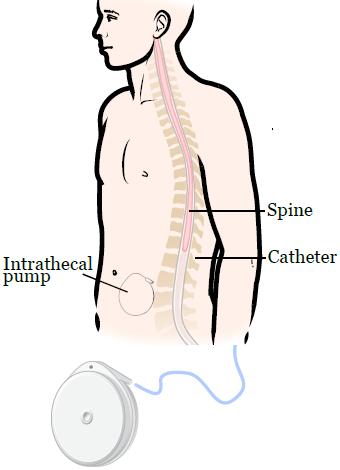
An intrathecal (in-truh-THEE-kul) pump is a small, round device that holds pain medicine. It’s implanted (surgically placed) under your skin at the side of your abdomen (belly).
This device sends pain medicine through a catheter (thin tube) right to the nerves in your spine. When the medicine goes right to the nerves in your spine, it lowers the amount of pain you feel.
Oral pain medicine is medicine you take by mouth. Intravenous (IV) pain medicine goes into a vein). If these pain medicines do not help your pain, your doctor may recommend an intrathecal pump.
Oral and IV pain medicine goes into every part of your body. This can cause side effects.
Most of the medicine from the intrathecal pump goes right to the nerves in your spine. This means you will need less medicine and should have fewer side effects.
The parts of your intrathecal pump
The intrathecal pump has 2 main parts: the pump and the catheter.
- The pump is a round device. It’s about 1 inch thick and 3 inches wide, about the size of a hockey puck. The pump will look like a bulge under the skin of your abdomen (see Figure 1).
- The catheter is connected to the pump. It sends pain medicine from the pump to your nerves.
Intrathecal pumps and epidural catheters
Intrathecal pumps are not the same as epidural catheters. Epidural catheters are what people get during childbirth. Both pumps give pain medicine right to the nerves in your spine, but there are some differences.
This table gives some examples of how intrathecal pumps and epidural catheters are different.
| Intrathecal pump | Epidural catheter |
|---|---|
| The pump is inside your body | The pump is outside of your body attached to a pole |
| Placed during surgery while you’re asleep | Placed by your pain doctor with some medicine to make you comfortable |
| Can be used at home | Cannot be used at home |
About your intrathecal pump placement
If an intrathecal pump is right for you, you will have a surgery to implant your pump. Your nurse will give you more information about your surgery and tell you how to get ready.
What to expect during your surgery
You will get general anesthesia (medicine to make you sleep) before your surgery starts. Once you’re asleep, your doctor will make an incision (surgical cut) in your abdomen where the pump will be placed. Your doctor will make another incision on your back.
One end of the catheter will be placed near the nerves in your spine. The other end of the catheter will be attached to the pump so that it can give you pain medicine. Your doctor will close your incision with sutures (stitches).
Your surgery will take 1 to 3 hours.
What to expect after your surgery
After your surgery, your incisions may be sore. You will get a prescription for pain medicine before you leave the hospital. Talk with your healthcare provider about possible side effects.
They will also tell you when you can switch to over-the-counter pain medicine. This is medicine you get without a prescription.
You will stay in the hospital for 3 to 4 days. Your doctor will choose the type and amount of medicine you will need to control your pain.
They will also show you how to use the pump and personal therapy manager (PTM). The PTM is a handheld programmer. You will use it to give yourself an extra dose of medicine, if you need it.
Your healthcare provider will give you an identification (ID) card that says you have an implanted device. Carry this card at all times while you have your intrathecal pump, both in the hospital and at home.
Activities after your surgery
For about 6 to 8 weeks after your surgery, follow these guidelines so your body can heal.
- Do not lift anything heavier than 10 pounds (about 4.5 kilograms).
- Do not bend over, such as picking up something from the ground.
- Do not twist your body, such as to crack your back.
- Do not expose your body to very hot or cold temperatures. This includes a sauna or ice bath.
Talk to your pain doctor about when you can go back to your normal daily activities.
Do not use a hot tub or go scuba diving when you have an intrathecal pump in place.
Follow-up appointment
You will have a follow-up appointment with your doctor and pain doctor 1 to 2 weeks after your surgery. Your doctor will take out your sutures during this appointment.
Caring for your intrathecal pump
Refilling your pump
Your pain doctor will need to refill the medicine in your pump every 4 to 6 weeks. You will need to make appointments with your pain doctor for your refills.
Call your pain doctor’s office 1 week before your refill appointment so they can order your medicine in time.
Between refills
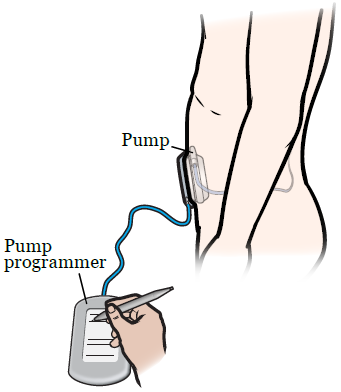
Between refills, the amount of medicine you get through your pump may need to change if your pain gets worse. Your pain doctor will adjust the settings on your pump with your pump’s programmer.
The pump programmer is a tablet used to change your pain medicine (see Figure 2). You must come to the clinic for refills and any changes to the pump.
If your pump is running low on medicine, it will make a beeping sound. This sound will alert your doctor.
What to expect at your refill appointment
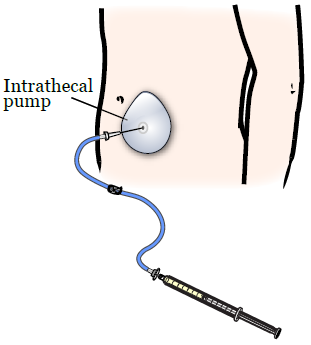
At your appointment, your pain doctor will numb your skin so that you will not feel any pain. Then, they will put a needle through your skin and into the pump. Your doctor will take out any medicine that is left in your pump. They will put new medicine into it (see Figure 3).
They will put a small bandage over the area where the needle was placed. Take the bandage off after 1 day.
Your doctor will give you a piece of paper with the following information each time your pump is refilled or changed:
- The kind of pain medicine that’s in your pump.
- The amount of medicine that the pump gives you.
- The date that your pump will need to be refilled with new medicine.
It’s important to keep track of this information so that your pump does not run out of medicine.
Your personal therapy manager
Your doctor will also give you a device called a personal therapy manager (PTM). This is a device you use to give yourself an extra dose of medicine from the pump if you need it. Your doctor will set the amount of medicine in this dose.
Keep your PTM fully charged. Your doctor will give you a charger for your device.
If you use the PTM, your pump refill date will show on the home screen. Your refill date may change depending on how many extra doses you use. Each time you use the PTM, the refill date will be updated on the home screen.
Remember to keep track of your new refill date. Call your pain doctor’s office 1 week before the new refill date to schedule an appointment. You will also need to let the office know to order the medicine.
Even with the pump and the PTM, you may still need to take oral pain medicine to control your pain.
Commonly asked questions
Will the intrathecal pump set off metal detectors?
In most cases, yes. It’s important to have your identification card with you to show to security.
Can I have magnetic resonance imaging (MRI) with the intrathecal pump in place?
Yes, but having an MRI will cause your intrathecal pump to stop working for a short time. It may sound an alarm while it’s stopped.
The pump should work normally after the MRI is done, or shortly after. If you’re having an MRI, tell your technologist that you’re using an intrathecal pump.
How long will the intrathecal pump work?
The battery in the intrathecal pump usually lasts 4 to 7 years. If the battery starts to wear down, it will alert your doctors when they program it. They will have enough time to replace the pump.
When to call your healthcare provider
Call your healthcare provider if:
- Your pain gets worse.
- Your side effects, like nausea or sedation (being sleepy), get worse.
- Your legs feel numb or weak.
- You have pain or redness at the pump site.
- You hear a beep from the pump.
- You have any questions or concerns.