This information describes your diagnostic laparoscopy (LA-puh-ROS-koh-pee).
About your diagnostic laparoscopy
Diagnostic laparoscopy is a minimally invasive procedure that lets your doctor see your organs. Minimally invasive procedures are done with small incisions (cuts).
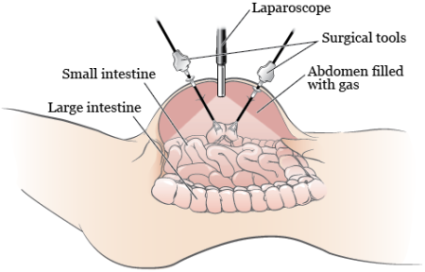
Your diagnostic laparoscopy is done by a surgeon. During your procedure, they will use a laparoscope and surgical tools. A laparoscope is a long, thin surgical tool with a video camera on the end of it. The surgeon will use the tools to:
- Look at the organs in your abdomen or pelvis to see if cancer cells have spread.
- Do a biopsy (a procedure to get tissue samples).
- Take washings (cell samples).
Your surgeon will make a small (1 to 2 inch) incision in your abdomen (belly) near your belly button. They will put the laparoscope through this incision. It will show a large picture of your organs on a television screen. This will let your doctor see the inside of your abdomen.
They will also make smaller incisions where they will put the surgical tools. After making the incisions, the surgeon will fill your abdomen with gas. The gas will push out the wall of your abdomen and move your organs away from each other. This gives them room to see and move the surgical tools during your procedure (see Figure 1).
Your surgeon may need to do a biopsy or take fluid samples during your laparoscopy. To do this, they will make a few more very small (about 5 to 12 millimeter) cuts. These incisions will be between the size of a pencil eraser and the end of an AAA battery. If they need to make a larger (open) incision, they will go over this with you before your procedure.
They may do your diagnostic laparoscopy with a robotic device. This is called a robotic-assisted laparoscopy. The robotic device holds the camera and other surgical tools. This helps your doctor control the tools to make precise surgical movements.
Your laparoscopy will be an outpatient procedure. This means that you can go home the same day. Most people who have a laparoscopy can start walking, eating, and drinking within 24 hours (1 day) of their procedure.
What to do before your diagnostic laparoscopy
Your nurse will give you information about your procedure. They will also give you a resource that explains how to get ready for your procedure.
Ask about your medicines
You may need to stop taking some of your usual medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking.
We’ve included some common examples below, but there are others. Make sure your care team knows all the prescription and over-the-counter medicines you take. A prescription medicine is one you can only get with a prescription from a healthcare provider. An over-the-counter medicine is one you can buy without a prescription.
It is very important to take your medicines the right way in the days leading up to your procedure. If you don’t, we may need to reschedule your procedure.
Anticoagulants (blood thinners)
A blood thinner is a medicine that changes the way your blood clots. Blood thinners are often prescribed to help prevent a heart attack, stroke, or other problems caused by blood clots.
If you take a blood thinner, ask the healthcare provider doing your procedure what to do before your procedure. They may tell you to stop taking the medicine a certain number of days before your procedure. This will depend on the type of procedure you’re having and the reason you’re taking a blood thinner.
We’ve listed some examples of common blood thinners below. There are others, so be sure your care team knows all the medicines you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Other medicines and supplements can change how your blood clots. Examples include vitamin E, fish oil, and nonsteroidal anti-inflammatory drugs (NSAIDs). Ibuprofen (Advil®, Motrin®) and naproxen (Aleve®) are examples of NSAIDs, but there are many others.
Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil. It will help you know which medicines and supplements you may need to avoid before your procedure.
Diabetes medicines
If you take insulin or other diabetes medicines, talk with the healthcare provider doing your procedure and the healthcare provider who prescribes it. Ask them what to do before your procedure. You may need to stop taking it or take a different dose (amount) than usual. You may also need to follow different eating and drinking instructions before your procedure. Follow your healthcare provider’s instructions.
Your care team will check your blood sugar levels during your procedure.
Weight loss medicines
If you take medicine for weight loss (such as a GLP-1 medicine), talk with the healthcare provider doing your procedure. Ask them what to do before your procedure. You may need to stop taking it, follow different eating and drinking instructions before your procedure, or both. Follow your healthcare provider’s instructions.
We’ve listed some examples of medicines that cause weight loss below. There are others, so be sure your care team knows all the medicines you take. Some of these are meant to be used to help manage diabetes but are sometimes prescribed just for weight loss.
|
|
Diuretics (water pills)
A diuretic is a medicine that helps control fluid buildup in your body. Diuretics are often prescribed to help treat hypertension (high blood pressure) or edema (swelling). They can also be prescribed to help treat certain heart or kidney problems.
If you take a diuretic, ask the healthcare provider doing your procedure what to do before your procedure. You may need to stop taking it the day of your procedure.
We’ve listed some examples of common diuretics below. There are others, so be sure your care team knows all the medicines you take.
|
|
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
What to do the day before your diagnostic laparoscopy
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
What to do the day of your diagnostic laparoscopyy
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
What to bring with you
Wear or bring loose-fitting, comfortable clothes to wear home. Your abdomen may be a little swollen or sore after your procedure.
What to expect when you arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having a procedure on the same day.
When it’s time to change, you’ll get a hospital gown, robe, surgical head covering, and nonskid socks to wear. You’ll need to remove any prosthetic devices, wig, and religious articles, if you have them.
Meet with an anesthesiologist
You will also meet with an anesthesiologist (A-nes-THEE-zee-AH-loh-jist). An anesthesiologist is a doctor with special training in anesthesia. They will give you anesthesia during your procedure. They will also:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your procedure.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Going into the procedure room
When it’s time for your procedure, you’ll remove your hearing aids, glasses, and dentures, if you have them. You’ll either walk into the procedure room or a staff member will bring you there on a stretcher.
Inside the procedure room
A staff member will take you into the operating room and help you onto the operating table. Your anesthesiologist will place an intravenous (IV) line into a vein, usually in your arm or hand. The IV line will be used to give you fluids and anesthesia during your procedure.
Your anesthesiologist will also monitor your heart rate and breathing throughout your procedure.
Once you’re asleep, your healthcare provider will place a catheter (thin, flexible tube) into your bladder to drain urine. They may also place a tube through your nose or mouth into your stomach to empty it. They will usually remove these in the operating room before you wake up.
Then, they will start your laparoscopy. Once they finish, your doctor will release the gas from your abdomen. They will close your incisions with sutures (stitches), Dermabond® (skin glue), or Steri-Strips™ (surgical tape).
What to do after your diagnostic laparoscopy
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your procedure. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
Caring for yourself at home
The following are general instructions to follow after your laparoscopy. If your doctor or nurse gives you different instructions from the ones below, follow the instructions they gave you.
- Rest on the day of your procedure. You will be drowsy from the anesthesia.
- Do not drink alcohol for 24 hours after your procedure.
- Do not drive a car for 24 hours after your procedure.
- Do not shower for 24 hours after your procedure.
- Starting 24 hours after your procedure, you can slowly start doing your usual activities again, depending on how you feel.
- Avoid strenuous activity for at least 1 week after your procedure. This includes activities such as lifting objects heavier than 10 pounds (4.5 kilograms).
Call your doctor’s office to schedule a follow-up appointment if you do not have one scheduled.
How to manage your pain
Pain after a laparoscopy is different for everyone. Pain from your incisions is usually mild and can last for several days. Many people have shoulder pain, which is a common side effect of expanding your abdomen. This can range from mild to severe (very bad) and may last for 7 to 10 days. Your healthcare provider will tell you what medications to take to manage your pain.
How to care for your incisions
You can take off the bandages covering your incisions 24 hours after your laparoscopy. You can shower after you take off the bandages. Leave your incisions exposed to the air to help them heal.
If you have Steri-Strips or Dermabond over your incisions, it will fall off by itself in 7 to 10 days. If you have stitches, they should dissolve on their own.
When to call your healthcare provider
Call your healthcare provider if you have:
- A fever of 101 °F (38.3 °C) or higher.
- Pain, even after taking medication to help.
- Redness around or drainage from your incision(s).
- Severe bloating or swelling in your abdomen.
More Resources
For more information, read: