This information explains what overactive bladder (OAB) is, the symptoms, and how to diagnose and treat it.
About your bladder
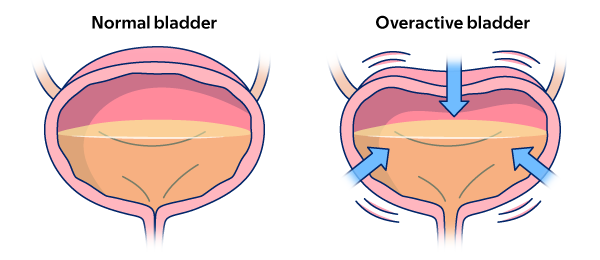
Your bladder is an organ that holds urine (pee). As urine flows into your bladder, the walls of your bladder stretch. This helps make room for more liquid.
When you urinate (pee), your bladder pushes urine out of your body through your urethra (yoo-REE-thruh). The urethra is the tube that carries urine from your bladder to outside your body. While this happens, the muscles in your urethra and pelvis relax.
What is OAB?
Overactive bladder is when the muscles in your bladder squeeze down too often, too strong, or both (see figure 1). This can cause urine to come out at the wrong time. This can be uncomfortable, embarrassing, and cause you to avoid social activities.
Causes and risk factors of OAB
As you get older, you may be more likely to have OAB. OAB can also be caused by:
- Bladder conditions, such as infection or pelvic floor muscle dysfunction. This is when the muscles that support the bladder and other organs do not work as well as they should.
- Certain health conditions, such as diabetes.
- Diet, such as eating or drinking things that irritate (bother) your bladder. These include caffeine, spicy foods, and carbonated (fizzy) drinks.
For some people, we do not know what causes OAB.
Symptoms of OAB
People with OAB may feel the urge to pee right away or pee often. This can happen even if their bladder is not full. They may leak urine or empty their whole bladder before they can get to the bathroom.
Symptoms of OAB include:
- Nocturia (nok-TOOR-ee-uh): Having to pee more than once while you’re sleeping.
- Urinary urgency incontinence (UUI): Leaking urine while having a sudden, strong urge to pee.
- Urinary frequency: Having to pee often, usually more than 8 times a day.
- Urinary urgency: Having a strong, sudden need to pee right away.
How to diagnose OAB
Talk with your healthcare provider, urogynecologist (YOO-ruh-GY-neh-KAH-loh-jist) or urologist (yoo-RAH-loh-jist) if you have symptoms of OAB.
- A urogynecologist is a doctor with special training in diagnosing and treating pelvic floor conditions, such as weak bladder.
- A urologist is a doctor with special training in diagnosing and treating urinary organs and urologic diseases. This includes pelvic floor conditions, such as weak bladder.
Your healthcare provider will do a physical exam. They will ask you when you leak urine, and how often. They may also order:
- Urodynamics (YOO-ruh-dy-NA-miks) tests to help them learn more about your bladder and urethra. A urodynamics test uses a catheter and manometer to measure the pressure in your bladder. Read Urodynamic Evaluation to learn more.
- Urine analysis tests to check for urinary tract infection (UTI) and blood in your urine.
- An ultrasound to see how much urine is in your bladder after you pee. Read About Your Transrectal Prostate Biopsy With Ultrasound to learn more.
Your healthcare provider may tell you to keep a bladder diary. They will ask you to record how much you urinate. You will record what you drink, how much, and how often. This will help them learn more about your bladder symptoms.
Treatments for OAB
Talk with your healthcare provider about which treatment or treatments for OAB are best for you.
Nutrition and diet
Some drinks can cause bladder spasms and make OAB symptoms worse. These include:
- Drinks with caffeine, such as coffee, tea, and soda.
- Drinks with fruit juice or artificial sweeteners.
- Drinks with alcohol.
Your healthcare provider can help you plan changes to your diet to ease the symptoms of OAB.
Physical therapy
Going to the bathroom often can cause your bladder to hold less urine. This can make you urinate even more often and make symptoms of OAB worse.
You can retrain your bladder by doing exercises to strengthen the muscles that help you hold in urine. Over time, this can help you go to the bathroom less often to urinate. It may take up to 3 months before you see results.
Talk with your healthcare provider to see if pelvic floor physical therapy is right for you. They may give you a referral for a pelvic floor physical therapist (PT) who can teach you these exercises.
Medicine
Your healthcare provider may prescribe medicine to help ease the symptoms of OAB. These medicines have different side effects. Talk with your healthcare provider about which medicine is right for you.
Botox
A Botox injection (shot) into your bladder wall can help to relax your bladder. This can help it hold more urine and ease the symptoms of OAB.
Your healthcare provider will give you local anesthesia (A-nes-THEE-zhuh) or sedation (seh-DAY-shun). Local anesthesia is medicine that numbs an area of your body. Sedation is when you’re calm, relaxed, or sleepy from medicine you get before your injection. Then, they will use a needle with a small camera on it to inject Botox into your bladder wall.
Some people may get a UTI or have trouble emptying their bladder after getting Botox. Talk with your healthcare provider about whether Botox is right for you.
Acupuncture
Acupuncture uses very thin needles at specific places on your body to relieve pain and other symptoms. An acupuncturist (AK-yoo-PUNK-cheh-rist) will put the needles into your skin at specific places on your body. An acupuncturist is a person who has special training in acupuncture.
Acupuncture can help relax bladder nerves and reduce urgency and leakage. It can also improve urinary symptoms, such as frequent nighttime urination. Read About Acupuncture to learn more.
Nerve stimulation
Nerve stimulation (nerv STIM-yoo-LAY-shun) is similar to acupuncture. Your healthcare provider will put a small needle into nerves that affect bladder function. They will use a device to send small impulses into the nerves. This changes the signals your nerves send to your bladder to help you need to urinate less often. Talk with your healthcare provider about whether nerve stimulation is right for you.
Low-dose vaginal estrogen
Low-dose vaginal estrogen often comes as a cream or tablet that you place in your vagina. It helps strengthen the tissues of the bladder and urethra. This can reduce urgency and frequent urination.
Manage nocturia
To help manage nocturia:
- Avoid drinking anything for 3 hours before bedtime.
- Urinate before you go to bed.
- Do not use any bladder irritants after 12 p.m. This includes coffee, tea, soda, and alcohol.
- Get tested for sleep apnea. Sleep apnea is when breathing stops during sleep. This can make OAB and nighttime urination worse. Treating sleep apnea can help your body make less urine at night and wake up less often to urinate.
Caring for your skin
For people with a vagina
All-cotton or incontinence pads, diapers, and incontinence underwear can help hold leakage. Incontinence pads are gentler on the skin than menstrual pads for people with a vagina.
Keep the skin around the vagina dry whenever possible. It may help to use a barrier cream, such as Aquaphor® or Vaseline®, can help.
For people with a penis
All-cotton or incontinence pads, diapers, and incontinence underwear can help hold leakage. Penile clamps may be helpful for people with a penis.
When to call your healthcare provider
If you think you have symptoms of a UTI, call your healthcare provider right away. This includes:
- Feeling burning when you urinate.
- Having urine that smells very bad.
- Having cloudy urine.
You should also call your healthcare provider if you have:
- A fever of 100.4 °F (38 °C) or higher.
- Blood in your urine when you pee.
- Trouble emptying your bladder.
- Other symptoms of overactive bladder.
- Body shaking.
- Chills.
- Confusion, if you are 80 years old or older.
