This information will help you get ready for your procedure to have a percutaneous endoscopic gastrostomy (PEG) feeding tube or a percutaneous endoscopic jejunostomy (PEJ) feeding tube placed at MSK.
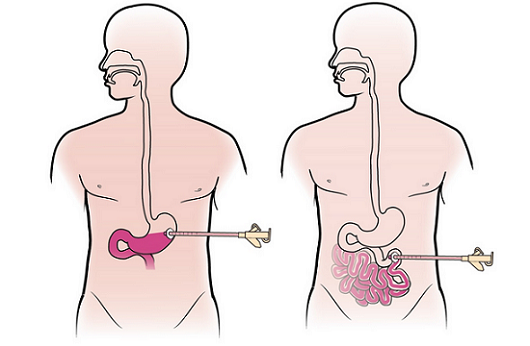
A PEG is a feeding tube that is placed into your stomach (see Figure 1, left). If the tube can’t be placed into your stomach, you may have a PEJ tube placed instead (see Figure 1, right). A PEJ tube is placed in your jejunum, which is the second part of your small intestine. The tube is placed during an endoscopy (a procedure that lets your doctor see inside your stomach and small intestine).
The feeding tube will give you nutrients if you’re not able to get enough through eating and drinking. If you’re able to eat, you can continue to do so after the PEG or PEJ tube is placed. You will use the tube to give yourself enough nutrition to meet your needs.
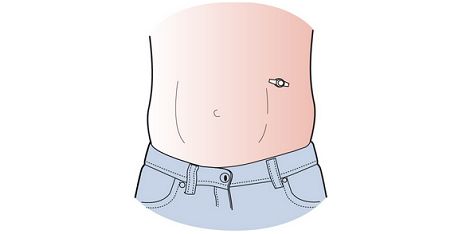
If you need long-term nutrition support, your doctor may convert your PEG into a low-profile gastrostomy button into your stomach (see Figure 2). Your doctor may convert your PEJ into a low-profile jejunostomy button into your small intestine. With both of these buttons, you will attach the feeding adapter to get nutrition.
1 week before your procedure
Speak with a registered dietitian
An outpatient registered dietitian will call you before your feeding tube is placed. They’ll ask you if you’re able to use your mouth to eat, what type of food you eat, and how much you’re eating. They’ll also talk with you about your tube feeding plan. This will include the type of formula you should use and how you will manage your feeds. They’ll teach you how to give yourself the formula through your feeding tube. They’ll follow up with you 1 to 2 days after your feeding tube is placed. This is to make sure you received all of your supplies and are tolerating your feedings.
Ask about your medications
You may need to stop taking some of your medications before your procedure. We have included some common examples below.
- If you take medication to thin your blood, ask the doctor who prescribes it for you when to stop taking it. Some examples are warfarin (Coumadin®), dalteparin (Fragmin®), heparin, tinzaparin (Innohep®), enoxaparin (Lovenox®), clopidogrel (Plavix®), and cilostazol (Pletal®).
- If you take insulin or other medications for diabetes, you may need to change the dose. Ask the doctor who prescribes your diabetes medication what you should do the morning of your procedure.
Get a letter from your doctor, if needed
If you have an automatic implantable cardioverter-defibrillator (AICD), you will need to get a clearance letter from your cardiologist (heart doctor) before your procedure.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
3 days before your procedure
You will get a call from a nurse in the Endoscopy Prep Lab. The nurse will review these instructions with you and ask you questions about your medical history. The nurse will also review your medications and tell you which to take the morning of your procedure.
The day before your procedure
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
If you need to cancel your procedure, call the GI scheduling office at 212-639-5020.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
The day of your procedure
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Things to remember
- Take the medications you were instructed to take the morning of your procedure with a few sips of water.
- Do not put on any lotion, cream, powder, deodorant, make-up, cologne, or perfume.
- Remove all jewelry, including body piercings.
- Leave all valuables such as credit cards and jewelry at home.
- If you wear contacts wear your glasses instead.
What to bring
- A list of the medications you take at home, including patches and creams.
- Medications for breathing problems (such as inhalers), medications for chest pain, or both.
- A case for your glasses or contacts.
- Your Health Care Proxy form, if you have completed one.
Where to go
Your procedure will take place at one of these locations:
David H. Koch Center
530 E. 74th St.
New York, NY 10021
Take the elevator to the 8th floor.
Endoscopy Suite at Memorial Hospital (MSK’s main hospital)
1275 York Ave. (between East 67th and East 68th Streets)
New York, NY 10065
Take the B elevator to the 2nd floor. Turn right and enter the Endoscopy/Surgical Day Hospital Suite through the glass doors.
Visit www.msk.org/parking for parking information and directions to all MSK locations.
What to expect
Once you arrive at the hospital, doctors, nurses, and other staff members will ask you to state and spell your name and date of birth many times. This is for your safety. People with the same or similar name may be having procedures on the same day.
Your doctor will explain the procedure to you and answer any questions you may have. They will ask you to sign a consent form (a form that says you agree to the procedures and understand the risks).
When it’s time for your procedure, you will be brought into the procedure room and helped onto an exam table. You will be attached to equipment to monitor your heart rate, breathing, and blood pressure. You will also receive oxygen through your nose. Your nurse will place a mouth guard over your teeth to protect them.
You will receive anesthesia (medication to make you sleepy) through your IV. Once you’re asleep, your doctor will pass the endoscope (a tube with a camera on it) through your mouth, down your esophagus (food pipe), into your stomach, and into the first part of your small intestine. Your doctor will check your stomach and small intestine before placing your PEG or PEJ tube.
Your doctor will make a tiny incision (surgical cut) on the skin of your abdominal (belly) wall and pass a feeding tube through the incision. The feeding tube will come out about 8 to 12 inches (20 to 30 centimeters) outside your body and will be covered by a small dressing (bandage) to keep it in place. When your doctor has finished the procedure, they will take out the endoscope.
After your procedure
In the hospital
You will be taken to the Post Anesthesia Care Unit (PACU), where your nurse will monitor your temperature, heart rate, breathing, and blood pressure. They will also check the bandage around your tube. You will stay in the PACU until you’re fully awake.
When you’re fully awake, your nutrition nurse practitioner (NP) will show you and your caregiver how to give yourself the feedings and care for your PEG or PEJ tube. It’s very important to have your caregiver with you during the teaching session. You’ll also receive a resource that explains how to give yourself feedings with your PEG or PEJ tube.
Your nutrition NP will go over possible side effects that you may experience with your feeding tube and will give you the HPN (Home Parenteral Nutrition) Complication Chart as a reference. This chart provides guidelines on how to treat possible complications. Call your doctor or NP if you’re having any problems.
You will also receive supplies for your feeding tube for the first few days before you leave the hospital. After that, your nurse will explain how you can order these from the company. The supplies include:
-
Supplies for dressing change:
- 4 x 4 gauze.
- Tape or Cath-Secure®
- Zinc oxide (Desitin®) ointment
- Iodine (Betadine®) swab sticks
- Syringe for flushing your tube with water
At home
- You may feel some soreness in your throat. This is normal and will get better in 1 or 2 days.
- You may have some discomfort at your incision site for the first 24 to 48 hours (1 to 2 days). If so, take your pain medication as instructed.
- You can shower 48 hours (2 days) after your procedure. Do not take tub baths or go swimming for 2 weeks after your procedure.
- You may see dark green or yellow drainage around your PEG or PEJ site. A small amount of green or yellow drainage is normal.
Caring for the skin around your PEG or PEJ tube
You will need to care for the skin around your PEG or PEJ tube. Follow the steps below.
Check your skin
Check the skin around your feeding tube every day. Look for any redness, swelling, or pus. Tell your doctor or NP if you’re having any of these symptoms.
Follow these instructions for the first 2 days after your procedure.
- Remove the old dressing.
- Clean the skin around the tube with iodine swab sticks once a day.
- Apply zinc oxide ointment.
- Cover the incision site with a 4 x 4 gauze.
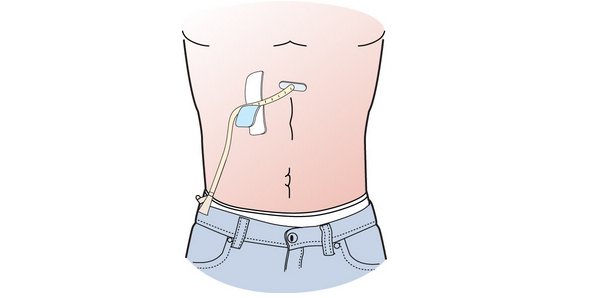
- Loop the tube (see Figure 4) and secure it with tape or use a Cath-Secure tab to hold it in place.
Check your skin in the shower
On the third day after your procedure, begin a daily routine of caring for the skin around your tube while showering.
- Before you shower, remove the old dressing around your tube.
- Wash the area with soap and water for at least 20 seconds. Gently pat it dry.
- After you get out of the shower, apply zinc oxide ointment.
- Cover your insertion site with a 4 x 4 gauze pad.
- Loop the tube and secure it with tape or with a Cath-Secure tab.
To protect your skin from your PEG or PEJ bumper, apply zinc oxide and gauze.
To protect your skin from secretions, change the dressing whenever it gets wet.
Flushing your tube or button
Flushing your PEG or PEJ tube
Flush your PEG or PEJ tube once a day or as directed by your doctor.
-
Gather your supplies:
- 60 mL syringe, either one with catheter tip or an ENFit syringe.
- 60 mL of water (room temperature or warm, plain tap water) in a cup.
- Paper towels.
- Wash your hands with warm water and soap for at least 20 seconds or use a hand sanitizer.
- Pull up 60 mL of water into the syringe.
- Place the paper towels under the Y-port at the end of the tube to absorb any drainage.
- Clamp the tube.
- Insert the syringe into the Y-port of the PEG or PEJ tube.
- Unclamp the tube and gently push the plunger to inject the water.
- Re-clamp the tube.
- Remove the syringe from the Y-Port of the PEG or PEJ tube.
- You can reuse your syringe. Rinse it in warm water and dry it with clean paper towels after each time you flush your tube.
If you’re having trouble flushing your tube, call your doctor or nurse.
Flushing your gastrostomy or jejunostomy button
Flush your gastrostomy or jejunostomy button once a day or as directed by your doctor.
-
Gather your supplies:
- 60 mL syringe, either one with catheter tip or an ENFit syringe.
- 60 mL of water (room temperature or warm, plain tap water), in a cup.
- Feeding tube adapter.
- Wash your hands with warm water and soap for at least 20 seconds or use a hand sanitizer.
- Pull up 60 mL of water into the syringe.
- Prime the adapter with water and then clamp it.
- Connect the adapter to your gastrostomy or jejunostomy button.
- Insert the syringe into the Y-port of the adapter.
- Unclamp the adapter and gently push the plunger to push in the water.
- Re-clamp the adapter.
- Remove the syringe from the Y-port of your adapter.
- Disconnect the adapter from your gastrostomy or jejunostomy button.
- You can reuse your syringe. Rinse it in warm water and dry it with clean paper towels after each time your flush your button.
If you’re having trouble flushing your button, call your doctor or nurse.
When to call your healthcare provider
Call your healthcare provider if you have:
- A fever of 100.4° F (38° C) or higher.
- Chest pain or shortness of breath.
- Severe abdominal (belly) pain.
- Diarrhea (loose or watery bowel movements).
- Nausea (feeling like you’re going to throw up) or vomiting (throwing up).
- Any dizziness or weakness.
- Bleeding that doesn’t stop.
- Pain at your incision site that doesn’t get better with medication.
- Trouble flushing your PEG or PEJ tube or button.
- Drainage around your insertion site that soaks 5 or more gauze pads per day.
- Any sign of redness, swelling, or pus around the tube.