This information explains what plantar fasciitis is. It also describes some of its common causes and symptoms, and how it can be treated.
About plantar fasciitis
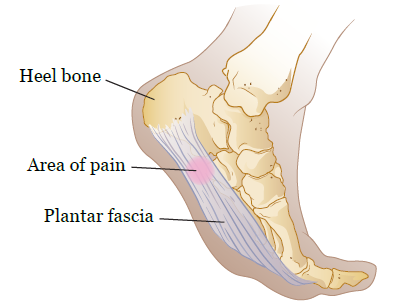
Your plantar fascia (PLAN-tar FA-shuh) is a thick band of tissue. It connects your heel bone to the ball of your foot (see Figure 1). Your plantar fascia acts like a rubber band that stretches with every step you take. It also supports the arch of your foot.
When you strain or hurt your plantar fascia, it can tear or become weak, painful, and swollen. This is called plantar fasciitis (fash-she-EYE-tis). It’s one of the most common causes of heel pain.
Symptoms of plantar fasciitis
Plantar fasciitis often feels like a burning, stabbing, or aching pain in the heel of your foot. Sometimes, the pain may go up to the ball of your foot. Most people with plantar fasciitis feel pain when they step out of bed in the morning.
You may also feel pain:
- After long periods of physical activity.
- At the end of the day.
- When standing after sitting for a while.
Causes of plantar fasciitis
There are many causes of plantar fasciitis, such as:
- Having tight calf muscles or Achilles tendons (the tough tissue that connects your calf muscles to your heel bone).
- Walking, standing, or running for long periods of time, especially on hard surfaces.
- Wearing shoes that do not fit well.
- Wearing shoes that do not have enough support.
- Having weak tissues in your feet due to aging.
- Having flat feet, high arches, or an uneven gait (an uneven way of walking).
- Being overweight.
- Pregnancy or hormonal changes. Hormones can cause ligaments and tissues to become more flexible than normal.
Diagnosis of plantar fasciitis
Your healthcare provider can often tell if you have plantar fasciitis based on your symptoms and a physical exam. They will check your feet and evaluate (look at) how you stand and walk. Sometimes, an X-ray or lab test may be done to rule out other possible problems.
Treatment for plantar fasciitis
There are treatments that can help ease the symptoms of plantar fasciitis. Your healthcare provider will make treatment recommendations based on your symptoms. The type of treatment you get depends on how long you’ve had your symptoms. It also can depend on how bad your symptoms are.
Although plantar fasciitis often goes away without causing any long-term problems, it can last from 6 to 18 months. You may need to take medicine to reduce pain and swelling. Your healthcare provider will tell you which medicine is best for you. You should always take medicine the way your healthcare provider tells you to.
Medicine
The most common types of medicine used are nonsteroidal anti-inflammatory drugs (NSAIDs). Examples of NSAIDs are ibuprofen (Advil® and Motrin®) and naproxen (Aleve®and Naprosyn®). NSAIDs should be taken with food.
Talk with your healthcare provider before taking NSAIDs if you:
- Have a history of gastrointestinal (stomach and intestines), liver, or kidney disease.
- Have a history of bleeding disorders.
- Are taking aspirin or any medicine that prevents your blood from clotting.
- Are taking corticosteroids (medicine that helps reduce swelling and inflammation).
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
Other treatments
Your healthcare provider may also suggest other treatments, such as:
- Taping your arches.
- Using night splints. These are support devices that protect your feet and stretch your feet while you sleep.
- Adding special aids in your shoes for extra support. This can be heel cups, orthotics (such as a brace or splint), or arch supports.
- Going to physical therapy.
If these treatments do not help, talk with your healthcare provider. They may suggest other treatments, such as corticosteroid injections (shots) or surgery.
How to ease plantar fasciitis pain
Here are some ways you can ease your plantar fasciitis pain:
- Place an ice pack wrapped in a towel on your heels. This will help reduce swelling and discomfort. Repeat up to 4 to 6 times every day for 10 minutes.
- Wear shoes that support your feet. Avoid wearing open-back shoes, sandals, high heels, flip flops, and walking barefoot.
- Take time to rest when exercising. Avoid standing, running, or walking for long periods of time.
- Rest your feet. Limit activities that put pressure on the heels and balls of your feet, such as running, jumping, and walking.
Exercises to ease plantar fasciitis pain
There are also some exercises you can do to help manage pain caused by plantar fasciitis.
Toe curls
You can do toe curls using a book or a towel. To do toe curls using a book:
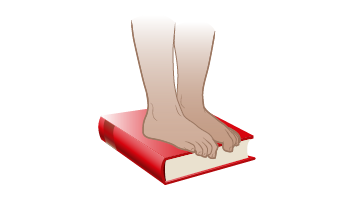
- Place a book on the floor and stand on top of it.
- Curl your toes around the edge of the book (see Figure 2). Then, straighten your toes.
- Repeat this movement for 2 minutes. Do this exercise 2 times every day.

To do toe curls using a towel:
- Place a towel on the floor and stand on top of it.
- Grip the towel under your toes (see Figure 3). Then, release.
- Repeat this movement for 1 to 2 minutes. Do this exercise 2 times every day.
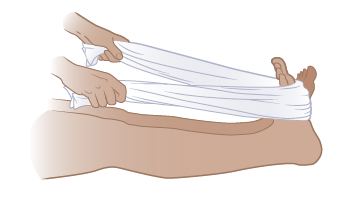
Foot stretches
You will need a towel for this exercise. Make sure it’s long enough to loop around your foot when you’re sitting with your legs straight (see Figure 4).
- Sit on the floor with your legs straight out in front of you.
- Loop the towel around your foot, keeping your leg straight out in front of you.
- Using the towel, pull the top part of your foot toward you (see Figure 4). You should feel stretching in your calf muscle.
- Hold this position for 10 to 30 seconds. Then, let go.
- Repeat this exercise 5 times in each session. Do 2 sessions every day.
Ankle circles
- Sit down in a chair and place your leg on a leg rest or on another chair.
-
Rotate your right ankle clockwise (to the right) 8 to 12 times (see Figure 5).
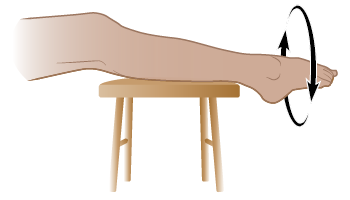
Figure 5. Ankle circles - Switch directions and rotate your right ankle counterclockwise (to the left) 8 to 12 times.
- Repeat this exercise with your left ankle.