This information will help you get ready for your tracheal (TRAY-kee-ul) or bronchial (BRON-kee-ul) stent placement at MSK. It also explains what to expect during and after your procedure.
About tracheal or bronchial stents
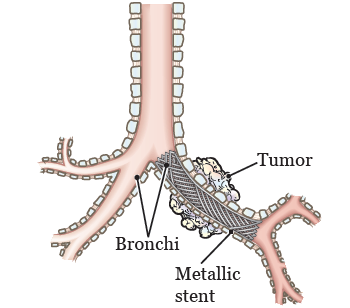
Many diseases or disease complications (problems) can narrow or block your airway. This can make you feel short of breath. A stent is a hollow tube that can be placed in your airway. It opens the narrowed area and helps you breathe (see Figure 1).
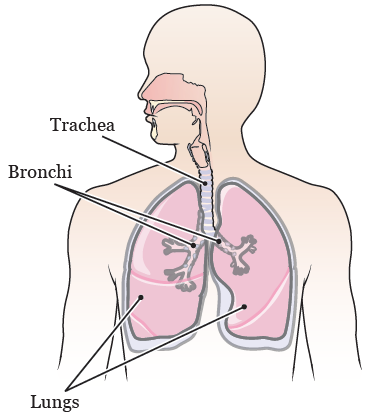
The stent can be placed in either your trachea (TRAY-kee-uh) or your bronchi (BRONG-ky). Your trachea (windpipe) is the tube that carries air from your nose and mouth into your lungs. Your bronchi are tubes that branch off your trachea and lead to different areas of your lungs (see Figure 2).
Stents come in different shapes and sizes. They can be made of different materials, such as metal or silicone. A computed tomography (CT) scan will help your doctor decide which type of stent will help you the most.
If you have a metal stent, it may not be safe to have a magnetic resonance imaging (MRI) scan. This is because metal and electronic devices can disrupt the MRI scanner’s magnetic field. If you have metal or electronic devices or objects in your body, tell the person doing your MRI. If an MRI is not safe for you, your doctor will order a different imaging test. If you have any other questions about your MRI, call your doctor’s office.
Your doctor will decide how long you will need the stent. At that time, they will remove the stent.
About your stent placement procedure
Your stent placement procedure will be done by an interventional pulmonologist (PUL-muh-NAH-loh-jist) or a thoracic (thor-A-sik) surgeon. These are doctors with special training in doing procedures to treat diseases in the lungs and chest.
Your stent will be placed during a procedure called a bronchoscopy (bron-KOS-koh-pee). Your doctor will put a bronchoscope (BRON-koh-SKOPE) though your nose or mouth, and into your trachea or bronchi.
A bronchoscope is a thin, flexible tube with a light and camera on the end of it. This will let your doctor see inside your airway while they’re placing the stent.
During the bronchoscopy, your doctor may do a biopsy. This is a procedure to take tissue samples from your lungs.
You will not have any incisions (surgical cuts) from your stent placement procedure. Most people go home the same day the stent is placed.
What to expect during your stent placement procedure
When it’s time for your procedure, you’ll go into the procedure room and be helped onto an exam table. Your healthcare provider will set up equipment to monitor (keep track of) your heart rate, breathing, and blood pressure. You will also get oxygen through a thin tube that rests below your nose.
Then, you will get anesthesia (medicine to make you sleep) through an intravenous (IV) line in your vein. Once you’re asleep, your doctor will insert (put) the bronchoscope into your nose or mouth. They will gently move it down the back of your throat and into your trachea or bronchi. Your doctor may also use fluoroscopy (live X-ray) to help guide them during your stent placement.
Once the bronchoscope is in the right place, your doctor will place the stent. They will put the stent into the bronchoscope and push it through to the end of the tube. When the stent comes out of the tube, it opens up. This pushes the walls of your airway open.
If your doctor needs to do a biopsy, they will do it during your procedure.
What to expect after your stent placement procedure
When you wake up after your procedure, you will be in the Post-Anesthesia Care Unit (PACU). A nurse will continue to monitor your heart rate, breathing, and blood pressure.
You may cough up a little blood after your procedure. This is normal. If you had a lung biopsy, you may have a chest X-ray to make sure your lung was not damaged. This type of injury is rare.
Your doctor will talk with you and the person taking you home after your procedure. They will explain how to take care of your stent.
Your doctor may prescribe oral or nebulized (NEH-byoo-lized) medicine. It helps prevent mucus buildup and keeps your stent clear.
Oral medicine is medicine you take by mouth, such as pills or tablets. Nebulized medicine comes in liquid form. Follow your doctor’s instructions for taking your medicine.
What to expect when you’re back home
Medicines
If your doctor prescribed oral or nebulized medicine, follow their instructions.
If you stopped taking any medicines before your procedure, follow your doctor’s instructions for starting them again.
Follow-up appointments
Your doctor’s office will call you to schedule a follow-up appointment. They will also schedule a follow-up bronchoscopy to look at your airway and stent.
Other information
- You can go back to doing your normal activities the day after your stent is placed.
-
While you have a stent, it’s safe to:
- Go through airport or security stations.
- Have radiation or chemotherapy.
Problems that can happen while you have a stent
Coughing or shortness of breath
Your stent is held in place by pressure. When swelling and redness from your procedure lessens, there’s a small chance your stent will move. This may lead to sudden coughing or shortness of breath. Very rarely, you may cough up the stent or a piece of the stent. If this happens, call your doctor right away.
Air flow that’s blocked by mucus or growing tissue
The inside of your stent can clog with mucus. This can block air flow. Depending on the type of stent, tissue can grow into the stent and make it narrow.
If your doctor prescribed oral or nebulized medicine, make sure to take it. Taking your medicine can stop these things from happening.
When to call your healthcare provider
Call your healthcare provider if:
- You have chest pain or pressure.
-
You cough up:
- More than 1 teaspoon (about 5 milliliters) of blood.
- Any amount of blood for more than 2 days after your procedure.
- The stent or a piece of the stent.
- The amount or color of your sputum (mucus that you cough up) changes.
- You have sudden shortness of breath or trouble breathing.
- You have a fever of 101 °F (38.3 °C) or higher.
- You start having bad breath that does not go away with normal oral hygiene (cleaning your mouth and teeth). Examples of normal oral hygiene are brushing your teeth and tongue, flossing your teeth, and using mouthwash.
- You have any problems, questions, or concerns.