This information explains implanted ports, port placement, and how to care for your port. In this resource, the words “you” and “your” refer to you or your child.
An implanted port is often called a port, mediport, or Port-A-Cath. A port protects your veins during cancer treatment.
What is an implanted port?
An implanted port is a type of central venous catheter (CVC). A CVC is a flexible tube that goes into one of your veins.
A port protects your veins from damage from repeated access. A port makes it easier for your care team to:
- Collect blood samples.
- Give you intravenous (IV) medication. This is medication that’s put into one of your veins. Some IV medications, such as anesthesia and some types of chemotherapy (chemo), must go through a large vein.
- Give you IV fluids.
- Give you IV blood products, such as platelets and plasma.
- Give you IV contrast. This is a special dye that helps your healthcare provider see your organs better.
Your care team can use your port to give you medication for several days in a row. You may need to get medication in a vein larger than the ones in your arms. Your port lets the medication go into your bloodstream through your vein.
Talk with your healthcare provider about whether getting a port is best for you and your treatment.
About your port placement
A surgeon or interventional radiologist (also called an IR doctor) will place your port in the operating room (OR). An IR doctor is a doctor with special training in image-guided procedures. They will place your port about 1 to 3 inches below your collarbone, depending on your size (see Figure 1). This helps your care team get easy access to your vein. If you wear a bra, your port will be about 1 inch from where your bra strap lies.
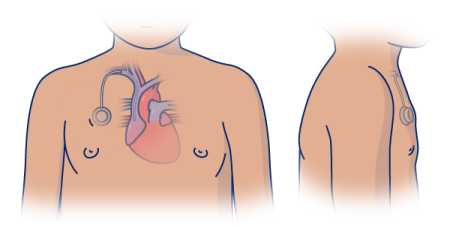
Your port may raise your skin about half an inch (1.2 centimeters). You may be able to feel it through your skin. Most people will not be able to tell that you have a port. Your port will not set off metal detectors.
Your port can stay in place for years. Your healthcare provider will remove your port when you don’t need it anymore. They also will remove it if it gets infected. You can have another port put in later, if you need one.
Parts of your implanted port
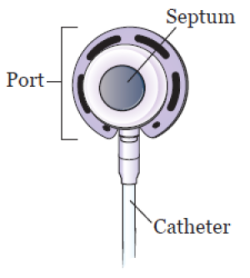
The parts of the implanted port are the port, septum, and catheter (see Figure 2).
Port and septum
The port is the starting point for fluids to flow through the catheter. It sits under your skin and has a raised center called a septum. This is the part of the port where needles will be placed. It’s also called the access point.
The septum is made from a self-sealing rubber material. Nothing can enter the port without a needle in it. The septum closes once the needle is removed.
Catheter
The catheter is a thin, flexible plastic tube. One end is connected to your port. The other end sits in your vein.
Types of implanted ports
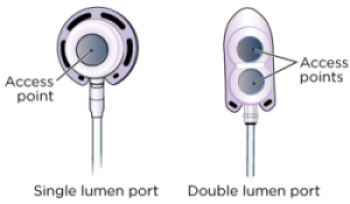
Ports can be shaped like a circle, oval, or triangle. Your port may be a mediport, BardPort®, PowerPort®, or Port-A-Cath. They can be a single lumen port or a double lumen port (see Figure 3). Your healthcare provider will choose the one that’s best for you and your treatments.
Single lumen port
A single lumen port has 1 access point. Most people get a single lumen port.
Double lumen port
A double lumen port has 2 access points. You can put a needle in each access point. You may get a double lumen port if you usually need more than 1 point of access for treatment.
Power-injectable ports
Most implanted ports are made to be used during imaging tests. These include computed tomography (CT) scans or magnetic resonance imaging (MRI). These ports let you have high speed injections (shots) of contrast. These are called power-injectable ports (see Figure 4).
Your healthcare provider will tell you if you have a power-injectable port. They will also give you a wallet card with information about your port. Carry this card with you at all times.

What to do before your port placement surgery
About 1 week before your surgery, you will meet with the pediatric surgery team for a pre-surgical visit. During this visit, they will teach you more about your new port and how to care for it. You should also have a family member or friend learn with you.
Ask about your medications
You may need to stop taking some of your medications before your surgery, including:
- Vitamin E
- Aspirin
- Anticoagulants (blood thinners)
- Insulin, or other medications for diabetes
Talk with your doctor about which medications are safe for you to stop taking.
If you’re taking any other medications, ask the doctor who prescribed them if you should stop taking them before your surgery.
If you take any medications in the morning, talk with your doctor about which medications you should take before your surgery. Your doctor may tell you to wait until after your surgery to take some of your medications.
Note the time of your surgery
A staff member will call you between and the day before your surgery. If your surgery is scheduled for a Monday, they will call you on the Friday before. If you don’t get a call by , call 212-639-5948.
The staff member will tell you what time to arrive at the hospital for your surgery. They will also remind you where to go.
How to get ready for your implanted port placement surgery
Your port placement surgery will take place in the operating room. Your healthcare provider will tell you how to get ready.
Take devices off your skin
You may wear certain devices on your skin. Before your surgery, some device makers recommend you take off your:
- Continuous glucose monitor (CGM)
- Insulin pump
Talk with your healthcare provider about scheduling your appointment closer to the date you need to change your device. Make sure you have an extra device with you to put on after your surgery.
You may not be sure how to manage your glucose while your device is off. If so, before your appointment, talk with the healthcare provider who manages your diabetes care.
Arrange for someone to take you home
You must have a responsible care partner take you home after your surgery. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your surgery.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
What to do the day before your port placement surgery
Shower with a 4% CHG solution antiseptic skin cleanser, such as Hibiclens
Shower with a 4% CHG solution antiseptic skin cleanser before you go to bed the night before your surgery.
- Wash your hair with your usual shampoo and conditioner. Rinse your head well.
- Wash your face and genital (groin) area with your usual soap. Rinse your body well with warm water.
- Open the 4% CHG solution bottle. Pour some into your hand or a clean washcloth.
- Move away from the shower stream. Rub the 4% CHG solution gently over your body from your neck to your feet. Do not put it on your face or genital area.
- Move back into the shower stream to rinse off the 4% CHG solution. Use warm water.
- Dry yourself off with a clean towel.
Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne after your shower.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your procedure. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their procedure.
What to do the day of your port placement procedure
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before procedures, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your procedure.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Instructions for medications
Take only the medications your doctor tells you to take the morning of your surgery. Take them with a small sip of water.
Things to remember
- Don’t put on any lotion, cream, powder, deodorant, makeup, powder, perfume, or cologne.
- If you wear contact lenses, wear your glasses instead. Wearing contact lenses during your procedure can damage your eyes.
- Don’t wear any metal objects. Remove all jewelry, including body piercings. The equipment used during your procedure can cause burns if it touches metal.
- Leave valuable items (such as credit cards and jewelry) at home.
- You will need to remove certain items before you go into the operating room. This includes hearing aids, dentures, prosthetic device(s), wig, and religious articles.
What to bring
- A case for your glasses, if you wear them.
- Loose, comfortable clothes to wear after your surgery.
- A small pillow or towel, if you’re traveling home in a car. You can use this to protect your incision (surgical cut) from the seatbelt.
- Your Health Care Proxy form and other advanced directives, if you completed them.
- Your medication, if you take any.
Where to go
Your surgery will take place at:
Presurgical Center (PSC)
1275 York Avenue (between East 67th and East 68th streets)
New York, NY 10065
Take the B elevator to the 6th floor.
Visit www.msk.org/parking for parking information and directions to all MSK locations.
What to expect when you arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having a surgery on the same day.
You will fill out a brief questionnaire if you have not already done so through MSK MyChart, the patient portal.
When it’s time to change for your surgery, you will get a hospital gown, robe, and nonskid socks to wear.
You will get sedation (medicine to help you feel calm) through a catheter. The catheter may be an IV in your arm or hand. It may also be a CVC, such as a peripherally inserted central catheter (PICC), if you already have one. A member of your care team will go over this with you before your surgery.
A staff member will bring you to the operating room when it’s time to place your port.
Meet with a nurse
You’ll meet with a nurse before surgery. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicines, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist (A-nes-THEE-zee-AH-loh-jist) will do it in the operating room.
Meet with an anesthesiologist
You’ll also meet with an anesthesiologist before surgery. They will:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your surgery.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Inside the operating room
Once you’re in the operating room, your healthcare provider will inject (give you a shot) of local anesthesia. Local anesthesia is medication to numb an area of your body. Your healthcare provider will inject the anesthesia into your neck and chest. You may also need general anesthesia to have your port placed. General anesthesia is medication to make you sleep during your surgery.
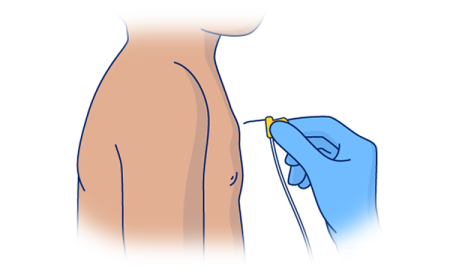
Your doctor will make a small incision (surgical cut) at the base of your neck (see Figure 5). It will be about 0.5 inches (1 centimeter) long. They will make a second small incision of about on your chest, under your collarbone. This incision will be about 1 to 1.5 inches (2.5 to 4 centimeters) long. Then, they will make a pocket under your skin. This will hold your port in place.
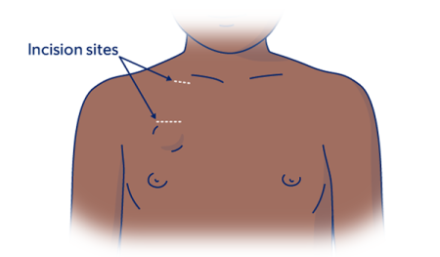
Your healthcare provider will place the catheter through the second incision and connect it to your vein.
Your care team will use sutures (stitches) or surgical glue called Dermabond® to close your incisions. If you have sutures, they will be absorbed into your body. You will not need to have them removed. They may also use Steri-StripsTM. These are short, thin strips of surgical tape that are stronger than a regular bandage.
Your surgery should take about 1 hour.
What to do after your port placement surgery
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your surgery. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
Tell your nurse if you’re feeling pain. They may give you medication for your pain.
Ask your nurse how long you can expect to stay in the PACU. Your care team will tell you when it’s safe to go home. You will need a responsible care partner to go with you.
Your nurse will take out your IV before you leave the hospital. They will explain how to change the bandage and care for yourself at home.
How to care for your incision site
You will have a bandage covering the small incision on your chest. You can take this bandage off 48 hours (2 days) after your surgery.
You may feel soreness or pain at your incision sites and where the catheter was tunneled under your skin. This should get better in 1 to 2 days. You can take over-the-counter pain medication (medication you get without a prescription) if you need it. You may also notice some bruising.
Wearing a seatbelt may put pressure on your incisions. You can put a small pillow or folded towel between the strap and your body to help with this.
Incisions closed with sutures
If your incisions were closed with sutures:
- You will have a small bandage covering each incision.
- Leave your bandages in place for 48 hours, or as long as your healthcare provider tells you to.
- Do not get your bandages wet. You can shower once your bandages are removed.
Incisions closed with Dermabond
If your incisions were closed with Dermabond:
- You may have small pieces of tape or bandages covering the incisions.
- Do not put lotion or adhesive on top of the tape or bandage.
- Do not pick or scratch the Dermabond. It will come off on its own after about 7 to 10 days.
- Your care team will give you instructions for how to shower safely until your incisions heal.
The skin over your port doesn’t need any special care. You can wash it as you normally would. If your care team used Steri-Strips, they will fall off on their own in 7 to 10 days.
Bathing and showering
- For the first 24 hours after your surgery, keep your bandage dry. You can take a sponge bath as long as your bandage doesn’t get wet.
- You can take a shower 48 hours (2 days) after your surgery. Don’t soak in a bathtub or pool. You can start taking baths 1 to 2 weeks after your surgery. Your doctor will tell you when this is. You can go completely underwater in a bathtub or pool as long as your port isn’t accessed.
-
If your port is accessed while you’re home:
- Cover the clear dressing over the port with a waterproof dressing (such as Aquaguard®). Your nurse can give you instructions for how to use it.
- Shower with Hibiclens every day to protect against infection. Follow the steps from the “Shower with a 4% CHG solution antiseptic skin cleanser” section of this resource.
- When washing, be gentle with your skin around the port site. You can wash gently with soap, but don’t use a washcloth or brush. Rinse your skin well and pat it dry with a soft towel.
- You can start using a washcloth during bathing and showering 2 weeks after your surgery. Avoid scrubbing the area until it’s completely healed. This is usually about 6 weeks after your surgery.
Physical activity after your surgery
Your healthcare provider will give you instructions on what exercises and movements you can do while your incisions are healing. Check with your healthcare provider before starting any exercises, such as:
- Gym class.
- Running.
- Stretching.
- Lifting anything over 10 pounds (4.5 kilograms).
- Contact sports, such as football.
Accessing your implanted port
Your healthcare provider will access your port when you need IV fluids or medication. They will do this by placing a needle through the access point (see Figure 6). The fluid or medication will move from your port through the catheter and into your bloodstream.
Only healthcare providers trained in port care should access your port.
Your care team may need to access your port the day it’s placed. If they do, they will put an access needle into the septum when your port is placed.
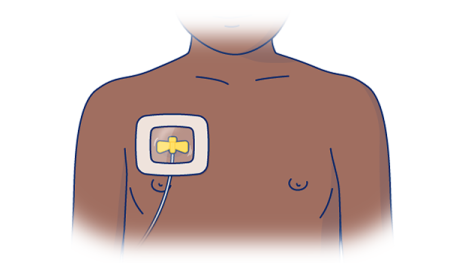
The needle and port will be covered by a special bandage any time your port is accessed (see Figure 7). The dressing will help to keep the needle in place. There also can be a small bandage over the top incision. You don’t need a bandage over your port when it’s not being used.
Flushing your implanted port
Your port flushes on its own while it’s being used. When it’s not being used, your port will need to be flushed at least every 12 weeks. Depending on when your appointments are, a nurse may flush your port more often. To do this, they will put a needle into your port. They will inject saline (sterile salt water) into your catheter. This is done to make sure the catheter does not get blocked. Your catheter may not work if it is blocked. If this happens, you may need to have your port removed.
Your will need to have your port flushed every 4 weeks when it’s not in use. This is to keep the catheter from getting clogged. A nurse at MSK will flush your port.
Removing your port
Your healthcare provider may remove your port when you no longer need it, or if it gets infected. Talk to your healthcare provider for more information about removing your port.
When to call your healthcare provider
Call your surgeon or IR doctor who did your surgery:
- If you have new or increased pain at the site of your port.
- If you have swelling or a growing bruise at the site of your port.
- If you have pus or fluid coming from your incision(s).
- If you notice your incision(s) are hot, tender, red, irritated, or opening.
- If you have a fever of 100.4° F (38° C) or higher.
- If you have chills.
Contact information
If you have any questions, contact a member of your care team directly. If you’re a patient at MSK call 212-639-2000 after , during the weekend, or on a holiday.
If an IR doctor placed your port, ask for the interventional radiology fellow on call.
If a surgeon placed your port, ask for the pediatric surgical fellow on call.