In patients with resected pancreatic ductal adenocarcinoma (PDAC), alterations in KRAS and TP53 were associated with worse outcomes, whereas alterations in homologous recombination deficiency (HRD) genes were associated with favorable prognoses, according to a study by our research team at Memorial Sloan Kettering Cancer Center (MSK). (1)
Our findings, published recently in Cancer, suggest that KRAS and TP53 variants, and HRD status should be studied further for their potential as biomarkers to inform prognoses and help guide treatment decisions. KRAS and TP53 alterations merit further study as therapeutic targets. (1)
We looked for associations between genomic alterations and clinical outcomes among 283 patients at MSK who underwent resection for PDAC between 2004 and 2017 and had sequencing results available from testing with MSK-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT™). (1)
Alterations in KRAS and TP53 were associated with worse overall survival (OS) than their respective wild types. The median OS for patients with KRAS mutations was 38.8 months versus 91.0 for wild type (p = 0.043). KRAS G12D alterations (alterations in KRAS codon 12) conferred the worst prognosis with a median OS of 31.6 months versus 39.2 months for other KRAS alterations (p = 0.012). (1)
For patients with TP53 mutations, median OS was only 37.4 months compared to 65.0 months for wild type (p = 0.035). TP53 truncations and loss of heterozygosity (LOH) conferred the worst prognoses. Patients with truncating alternations had a lower median OS of 33.9 months compared to 39.6 months for patients without truncating alterations (p = 0.02). Patients with TP53 mutations in regions with LOH had an even lower median OS of 26.6 months versus 39.2 months for those without LOH (p = 0.048). (1)
The median OS for patients with germline alterations in HRD genes (genes that lack the ability to repair DNA) was not reached, compared to 37.0 months (p = 0.35) for those without HRD mutations. (1)
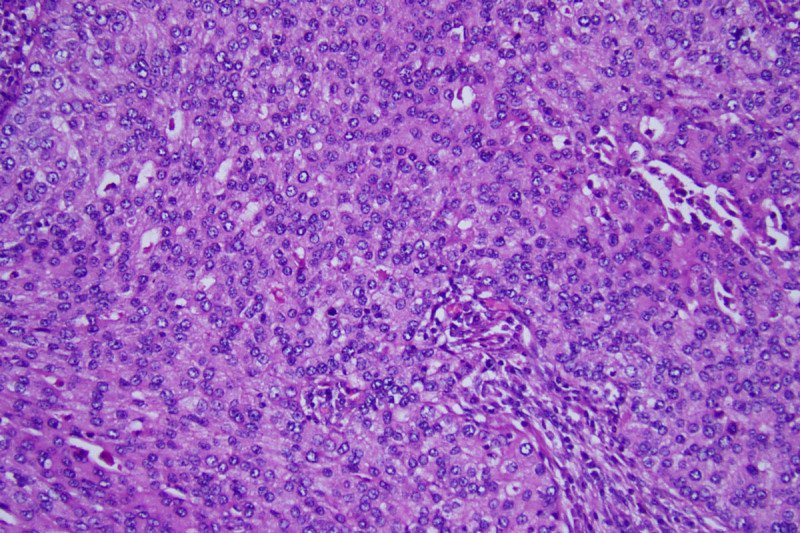
Pancreatic Adenocarcinoma
PDAC is estimated to become the second leading cause of cancer deaths by 2030. (2) It has a poor prognosis with an overall five-year survival rate of less than 10 percent. (3) Most patients present with locally advanced or metastatic disease: Only 15 to 20 percent have resectable disease at diagnosis. (4)
The genomic landscape for PDAC has been well characterized over the last decade, with KRAS, TP53, CDKN2A, and SMAD4 identified as the main alterations driving tumor growth. (5), (5),(7), (8)KRAS and TP53 mutations have been found in about 90 percent and 75 percent of cases, respectively. (9), (10), (11) Alterations in KRAS and CDKN2A occur early in tumorigenesis, whereas mutations in TP53 and SMAD4 occur in later stages. (12), (13) Scientists have also identified other genes involved in multiple oncogenic pathways, which are mutated at a lesser frequency. (5), (6), (7), (8) A growing number of studies have demonstrated that increasing numbers of driver genes are associated with poorer OS and recurrence-free survival (RFS) after resection for PDAC. (14), (15), (16)
Despite this increased understanding of the genomic landscape, relatively few clinically actionable mutations have been identified. Many targeted therapies are under investigation, but few have been validated. (17)– (18), (19), (20), (21) Several studies suggest that patients with germline BRCA1 and BRCA2 mutations experience improved outcomes with platinum-based chemotherapy and poly adenosine diphosphate-ribose (PARP) inhibitors. (8), (22), (23), (24), (25) However, no targeted agents against any of the four driver genes have been validated, and the U.S. Food and Drug Administration has not approved any drugs for use in the PDAC setting.
Study Design
We compared clinical outcomes with pathological data for 283 patients with PDAC who underwent resection at MSK between January 2004 and August 2017, and for whom we had sequencing results available in our prospectively collected genomic database.
MSK-IMPACT performs deep, targeted sequencing on all exons and selected introns of up to 468 cancer-related genes. The platform also tests for up to 88 cancer predisposition genes. Patients in our cohort had consented to have their primary tumors sequenced with MSK-IMPACT (NCT01775072) as part of clinical practice. (26) DNA was extracted from blood samples for somatic mutation calling and for a subset of 154 patients who had consented to germline analysis.
Given the recently emerging data on the use of platinum-based agents and PARP inhibitors to treat PDAC, we evaluated outcomes for patients with both germline and somatic alterations in HRD genes. We analyzed several HRD genes, including ARID1A, ATM, BAP1, BARD1, BLM, BRCA1, BRCA2, BRIP1, CHEK2, FAM175A, FANCA, FANCC, NBN, PALB2, RAD50, RAD51, RAD51C, and RTEL1.
Finally, we examined the mismatch repair (MMR) genes MLH1, MSH2, MSH6, and PMS2, and compared the mutational frequencies in this cohort with a larger group of both primary and metastatic PDAC tumors sequenced with MSK-IMPACT (n = 1,702).
Study Findings
Among the 283 patients, 58 (20 percent) had received neoadjuvant therapy, 205 (72 percent) underwent pancreaticoduodenectomy, and 218 (77 percent) had received adjuvant therapy. Most patients (81 percent) had their primary tumors sequenced before they received systemic treatment. The median OS for the entire cohort was 39.0 months (95% CI, 33.3–46.3 months), and the median RFS was 12.8 months (95% CI, 11.7–15.5 months). The most common site of disease recurrence was the liver and three-year cumulative incidence of recurrence (CIR) was 27.9 percent. (1)
KRAS was altered in 262 patients (93 percent), and among this group, 109 patients or 42 percent had G12D mutations. Mutations in TP53 occurred in 203 patients (72 percent), of which 54 patients (27 percent) had truncating mutations, and 80 (39 percent) had alterations in the presence of LOH. Truncating mutations and LOH co-occurred in only ten percent of patients (n = 29). ARIDIA, RNF43, and PTPRT were altered in more than five percent of the total patient cohort. A total of 47 patients had somatic HRD mutations, and only four patients had somatic alterations in MMR genes. (1)
The median OS for KRAS mutations was 38.8 months (95% CI, 33.0–45.5 months) versus 91.0 months for wild-type (95% CI, 34.9–not available, p = 0.043). KRAS mutations were associated with larger tumors and distant recurrences after resection. KRAS G12D alterations conferred the worst prognosis among KRAS alternations: median OS was 31.6 months (95% CI, 25.3–45.5 months) versus 39.2 months (95% CI, 37.4–75.2 months, p = 0.012) for all others. (1)
TP53 mutations were also associated with worse outcomes: median OS was 37.4 months (95% CI, 32.1–42.8 months) compared to 65.0 months for wild-type (95% CI, 33.0–not available, p = 0.035). Patients with TP53 truncating mutations had a decreased survival: median OS was 39.6 months (95% CI, 32.4-75.2 months) vs 33.9 months (95% CI, 24.0-39.0 months; p = .020). Those with associated LOH also had decreased survival with a median OS of 26.6 months (95% CI, 21.6-44.2 months) vs 39.2 months (95% CI, 34.5-49.1 months; p = 0.048), although there was no significant difference in RFS. (1)
We conducted univariate and multivariate analyses to look for an association between KRAS and TP53 status with OS in the setting of other potential confounders. Univariate analysis showed that KRAS mutations, TP53 alterations, stage III/IV tumors, lymphovascular invasion, and neoadjuvant therapy were associated with OS. However, when we adjusted for potential confounders, KRAS was no longer associated with OS, yet TP53 alterations remained significantly associated with a worse prognosis (hazard ratio 1.54; 95% CI, 1.01–2.33, p = 0.042). (1)
Genomic alterations were also associated with time to the site of first recurrence. The three-year CIR with TP53 truncations was 25.6 percent versus 10.4 percent without truncations (p = 0.009). The three-year CIR with simultaneous local and distant recurrences was 22.2 percent for TP53 mutations associated with LOH versus 9.1 percent without (p = 0.30). (1)KRAS mutations were associated with an liver recurrences: three-year CIR was 42.4 percent (95% CI, 23.9–35.6 percent) versus 5.8 percent (95% CI, 0.3–24.5 percent, p = 0.013), as were TP53 LOH, with a three-year CIR of 40.5 percent (95% CI, 29.0–51.7 percent) versus 24.5 percent (95% CI, 16.6–33.1 percent, p = 0.017). (1) Co-occurring KRAS/TP53 alterations trended toward significance. (1)
Patients with germline HRD alterations experienced significantly better survival compared to patients without them: median OS was not reached for those with the alterations compared to 37.0 months (95% CI, 33.0–49.8 months, p = 0.35) for those without. Interestingly, for somatic HRD mutations, we found no survival differences or with the use of platinum-based agents. However, the number of patients with somatic HRD mutations was small (17 percent). Larger studies may reveal differences in the future. (1)
Clinical Trials Testing Targeted Therapies in PDAC
KRAS is commonly mutated in other solid tumors. A recent U.S. phase I trial testing AMG 510, a small molecule inhibitor of KRAS G12C, showed a promising signal: patients with the mutation in colorectal and non-small cell lung cancers showed a partial response or stable disease. (27)
An initial phase I/IIa trial by researchers in Israel evaluated siG12D-LODER, a particle that releases RNA interference against KRAS G12D, and to a lesser extent, KRAS G12V, in combination with gemcitabine. The results showed a partial response or stable disease in all patients. (28)
MSK is currently participating in an ongoing randomized phase II trial evaluating gemcitabine and nab-paclitaxel with or without siG12D-LODER in patients with unresectable, locally advanced pancreatic cancer (NCT01676259). A capsule containing siG12D-LODER is inserted directly into the tumor via ultrasound-guided endoscopy every three months until response is observed.
At MSK, we are dedicated to using the latest genomic tools, clinical research, and treatments to improve outcomes for patients with PDAC. In total, we are currently conducting 23 clinical trials for PDAC to test a range of new treatment approaches, including novel targeted agents, immunotherapies, cancer vaccines, armed, activated T cells, and radiation approaches. We also have an ongoing pancreatic tumor registry, which we will help us study whether there are lifestyle or other factors that predispose patients to a higher risk of disease, determine if it is feasible to follow them with increased surveillance, and identify genetic risk factors.
This study was funded by the P30 Cancer Center Support Grant CA0008748, the David M. Rubenstein Center for Pancreatic Cancer Research, and the Reiss Family Foundation.
Eileen M. O’Reilly reports research funding to Memorial Sloan Kettering from Genentech-Roche, Bristol-Myers Squibb, Celgene, MabVax Therapeutics, BioAlta, AstraZeneca, and Silenseed and consulting/advisory roles with AstraZeneca, CytomX Therapeutics, BioLineRx, Targovax, Rafael Therapeutics, Celgene, Bayer, Polaris, Sobi, Silenseed, Ipsen and Merck. For disclosures from other authors, please refer to the paper.