Early CD4+ T cell reconstitution predicted non-relapsing mortality and overall survival (OS) in pediatric patients who received an allogeneic hematopoietic stem cell transplant (HCT) and developed acute graft-versus-host disease (GVHD), according to our research published recently in the journal Blood.
The findings suggest that patients with inadequate CD4+ immune reconstitution who develop acute GVHD may benefit from individualized treatment strategies, such as prolonged prophylaxis or more aggressive therapy, to improve their odds of survival.
In our dual center analysis, we retrospectively studied outcomes for 591 patients who received an allogeneic HCT at MSK Kids (315 patients), or the Wilhelmina Children’s Hospital or the Princess Máxima Center for Pediatric Oncology (UMC/PMC) in Utrecht, the Netherlands (276 patients). We examined non-relapse mortality and OS and stratified results by whether CD4+ T cell reconstitution achieved or did not achieve a threshold level of 50 cells/uL within 100 days after HCT or before the onset of acute GVHD. (1)
For patients with severe acute GVHD (grades III-IV) with or without threshold CD4+ T cell reconstitution within 100 days after HCT, non-relapse mortality was 5 percent versus 67 percent (p = 0.02) at MSK Kids and 30 percent versus 80 percent (p = 0.02) at UMC/PMC. In both cohorts, OS was inferior for patients with inadequate versus adequate CD4+ T cell reconstitution before the onset of acute GVHD: 33 percent versus 75 percent (p = 0.12) at MSK Kids and 20 percent versus 61 percent (p = 0.04) at UMC/PMC. (1)
Thus, early CD4+ T cell reconstitution is a simple, robust marker predictive of outcomes after HCT. These results were striking, given that they were similar for two independent centers using distinct transplantation strategies: UMC/PMC exclusively performed T replete HCT, and MSK Kids performed both T replete and ex vivo T cell depleted HCT.
Survival for children with malignant and non-malignant blood disorders, including cancer, has increased over time. For example, the five-year survival rate is now about 90 percent for children with acute lymphocytic leukemia (ALL) and about 65 to 75 percent for children with acute myelogenous leukemia (AML). (2) Still, treatment by experts at a high-volume center pioneering translational research confers significant benefits.
Acute Graft-versus-Host Disease
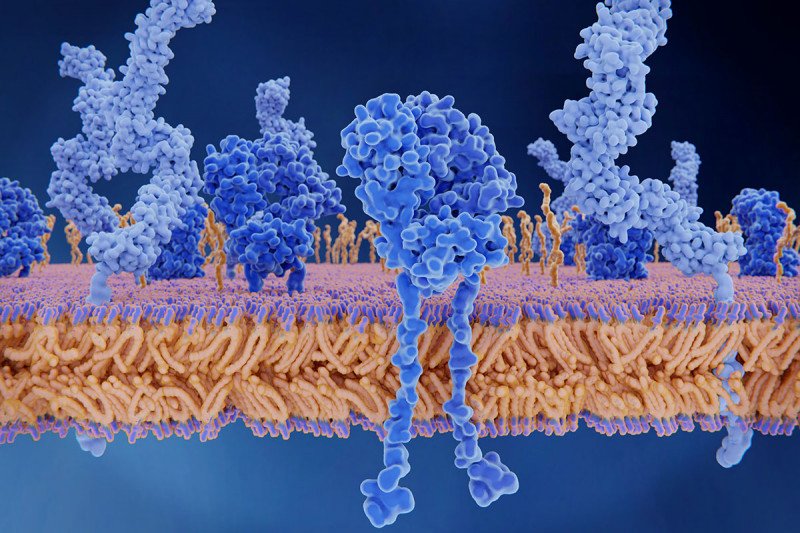
Acute GVHD is a life-threatening complication that may arise after allogeneic (from another person) HCT. It is caused by reactive donor lymphocytes recognizing a patient’s cells as foreign, due to minor histocompatibility antigens or major histocompatibility antigens in the case of HLA-mismatched transplants, and attacking them. (3)
All HCT protocols contain some method of prophylaxis, including medications administered after HCT to limit the risk of acute GVHD. (4) Some protocols also include serotherapy (antithymocyte globulin or alemtuzumab) or give cyclophosphamide after HCT for in vivo T cell depletion. (4), (5), (6), (7), (8) Still, acute GVHD is common, affecting 20 to 60 percent of patients receiving an allogeneic HCT, depending on patient characteristics and treatment protocols. (9)
Alternative strategies for preventing GVHD in human leucocyte antigen (HLA)-disparate HCTs include in vivo T cell depletion with post-transplant cyclophosphamide targeting rapidly activated alloreactive T cells and ex vivo T cell depletion with techniques such as CD34+ selection or the more recent alpha-beta T cell depletion method. Patients receiving T cell depleted transplants have a lower incidence of acute GVHD of 20 to 30 percent, but mortality rates remain high when treatments for acute GVHD fail. A recent review found that acute GVHD still accounts for 10 to 20 percent of deaths after allogeneic HCT. (10)
In our previous research, we demonstrated that early CD4+ T cell reconstitution predicts survival after HCT in a range of transplantation platforms. (11), (12), (13) CD4+ T cell reconstitution also overcomes the risk associated with viral reactivation with Epstein-Barr virus and human herpesvirus 6. (12)
Study Design: Patient Treatment and Immune Monitoring
For our present study, we looked for an association between CD4+ T cell reconstitution and survival probability after the onset of acute GVHD by evaluating data from patients receiving their first allogeneic HCT at two separate pediatric transplantation centers: MSK Kids in New York City between 2008 and 2017, and the Wilhelmina Children’s Hospital or the Princess Máxima Center for Pediatric Oncology (UMC/PMC) in Utrecht, the Netherlands between 2004 and 2017. Immune monitoring and clinical outcome data were recorded and registered prospectively. (1)
All patients were treated in particle-free, air-filtered, positive-pressure isolation rooms. Transplant specialists treated patients with conditioning regimens according to center-specific protocols. Patients at both centers received infection prophylaxis, and patients at UMC/PMC received selective gut decontamination. (1) At MSK, GVHD-prophylaxis consisted of either in vitro T cell depletion (with or without ATG) or calcineurin inhibitor-based prophylaxis combined with methotrexate for recipients of bone marrow and combined with mycophenolate mofetil for cord blood transplant recipients. At UMC/PMC, GVHD-prophylaxis consisted of cyclosporin A combined with either prednisolone for recipients of cord blood or methotrexate for recipients of bone marrow. (1)
Patients who developed acute GVHD grades II to IV were treated with methylprednisolone as first-line therapy. Refractory patients received “best available treatment,” which was mostly mesenchymal stromal cells, but other therapies such as antibodies and mycophenoloate mofetil were used when mesenchymal stromal cells were unavailable. Transplant teams at both centers monitored patients’ absolute numbers of CD4+ T cells. (1)
We examined the association between non-relapse mortality and OS with the presence or absence of adequate CD4+ T cell reconstitution, with adequate reestablishment defined as two measurements of CD3+CD4+CD8- ≥ 50 cells/uL within the first 100 days post-transplantation, or before the onset of acute GVHD, in line with previous studies. (11), (12), (14), (15) GVHD was classified according to the Glucksberg and Shulman criteria. (16), (17) Non-relapse mortality was defined as death due to a cause other than malignancy relapse within five years of follow-up. OS was defined as the time from transplantation to death or last follow-up, with a minimum follow-up of one year. (1)
Study Results
We included data from a total of 591 patients in our study: 315 at MSK Kids and 276 at UMC/PMC. The median age was 10.4 years (range 0.1–35.6) at MSK Kids and 7.1 years (range 0.2–22.7) at UMC/PMC. The incidence of acute GVHD grades II-IV was similar in both cohorts, affecting 70 patients (22.2 percent) at MSK Kids and 73 patients (26.4 percent) at UMC/PMC. The incidence of severe acute GVHD grades III-IV was also similar between centers, affecting 32 patients (10.2 percent) at MSK Kids and 29 patients (10.5 percent) at UMC/PMC. The median time to acute GVHD was 55 days at MSK Kids and 35 days at UMC/PMC. (1)
Multivariate analysis found that CD4+ T cell reconstitution predicted non-relapse mortality and OS in patients with moderate to severe acute GVHD. Note that adequate immune cell reconstitution did not decrease the risk of developing acute GVHD but was associated with improved outcomes compared to inadequate immune cell reconstitution. Patients with acute GVHD (grades II-IV) achieving CD4+ T cell reconstitution within 100 days after HCT had survival and non-relapse mortality comparable to patients who did not have acute GVHD: For patients treated at MSK Kids, non-relapse mortality was 5 percent versus 9 percent (p = 0.99), and OS was 61 percent versus 76 percent (p = 0.43), with and without immune reconstitution, respectively. For UMC/PMC patients, non-relapse mortality was 21 percent versus 18 percent (p = 0.65), and OS was 63 percent versus 76 percent (p = 0.19), with and without immune reconstitution, respectively. (1)
Looking at the subset of patients with severe acute GVHD (grades III-IV), CD4+ T cell reconstitution was associated with a significantly decreased non-relapse mortality of 5 percent versus 67 percent (p = 0.02) at MSK Kids and 30 percent versus 80 percent (p = 0.02) at UMC/PMC. This lower non-relapse mortality was associated with a trend to higher OS in the MSK Kids cohort of 75 percent versus 33 percent (p = 0.12) and significantly improved OS of 61 percent versus 20 percent (p = 0.04) at UMC/PMC. (1)
Finally, we performed a time-to-event analysis to evaluate the predictive value of CD4+ immune reconstitution before acute GVHD diagnosis on survival after acute GVHD. Due to limited data in the first few weeks after HCT from MSK Kids, we examined data from the UPC/PMC cohort. CD4+ immune reconstitution before developing severe acute GVHD (grades III-IV) was an even stronger predictor of outcomes: non-relapse mortality was 12 percent versus 74 percent (p < 0.001)and OS was 78 percent versus 24 percent (p < 0.001) for patients with and without CD4+ T cell reconstitution, respectively. (1)
In conclusion, our findings suggest that patients undergoing allogeneic HCT who do not achieve CD4+ immune reconstitution before developing acute GVHD might benefit from prolonged prophylaxis or more aggressive therapy to treat this life-threatening complication. Optimizing individualized conditioning regimens is essential for improving and predicting immune reconstitution.
Advancing Outcomes After HCT
There are several promising approaches for improving CD4+ T cell reconstitution after transplant currently being studied in prospective trials. One that can be performed across transplant platforms is individualizing the dosing of ATG and fludarabine. (18), (19) Other strategies involve low dose IL-2 therapy and infusion of graft-derived or third-party regulatory T cells. (20), (21), (22)
MSK Kids recently participated in a multicenter clinical trial using mesenchymal stromal cells to treat GVHD in children and adolescents (NCT00759018), published in May 2020. (23) We are currently conducting several clinical trials aimed at improving transplant outcomes and decreasing the risk of GVHD. For example:
- a trial that uses antibodies instead of chemotherapy as cytoreduction for patients with severe combined immune deficiency (SCID)
- and a trial of genetically engineered autologous stem cells for patients with sickle cell disease.
These include trials of a novel combination of chemotherapy agents combined with cord blood transplant (20-480) a novel approach to CD34+ selected transplantation to improve immune reconstitution by using individualized dosing (20-042).
The study was supported by the Children Cancer-free Foundation (KiKa) project number 142. All authors declared no competing interests.