Proton beam radiotherapy resulted in similar oncologic outcomes with less toxicity and improved quality of life than photon beam radiotherapy (intensity modulated radiotherapy, IMRT) in patients with head and neck cancers, according to results of an MSK-led clinical trial presented today at the 2025 American Society for Radiation Oncology Annual Meeting: Rediscovering Radiation Medicine and Exploring New Indications (ASTRO 2025).
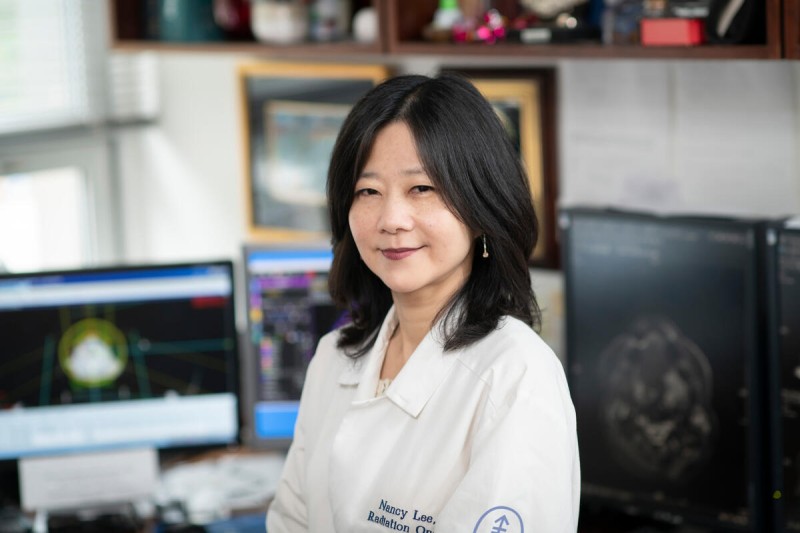
“Until this study, prospective evidence comparing proton beam radiotherapy with IMRT for this patient population had been lacking,” said radiation oncologist and early drug development specialist Nancy Lee, MD, Service Chief of Head & Neck Radiation Oncology and Proton Therapy at MSK, who designed and initiated the trial. “Importantly, our study included patient-reported outcomes as clinician grading alone tends to underestimate symptom burden.”
Study Rationale and Design
For many salivary gland, melanoma, and skin cancers of the head and neck, anatomic complexity makes it challenging to determine the optimal post-operative radiotherapy approach.
While the advent of IMRT has improved conformality and reduced late effects, acute toxicities remain common, with many patients experiencing declining quality of life and requiring intensive supportive care. Proton beam radiotherapy has the potential to reduce dose distributions to normal tissues while maintaining tumor control similar to IMRT.
Dr. Lee designed and initiated the phase 2 clinical trial (NCT02923570), which took place at nine locations, including seven MSK locations in New York and New Jersey, as well as the Baptist Health Miami Cancer Institute in Miami, a member of the MSK Cancer Alliance, and the Mayo Clinic in Rochester.
Eligible patients with salivary gland tumors, skin cancer, melanoma, and tonsil cancer for whom post-operative unilateral radiation is the standard-of-care were randomized to receive proton or photon radiotherapy. High-risk regions received 60 to 66 Gray (Gy) and lower-risk areas received 50 to 54 Gy.
The primary endpoint of the study was whether the physician-reported rate of acute grade 2 or higher mucositis was lower with proton beam versus IMRT, according to the Common Toxicity Criteria Adverse Event (CTCAE) v4.03, assessed from the start of radiation until three months post-treatment.
The secondary endpoints were as follows: other acute and late toxicities; patient-reported outcomes (PRO-CTCAE); local, regional, and distant metastasis progression-free intervals; progression-free survival (PFS); and overall survival (OS) between the two radiotherapy technologies.
Study Results
Edward Christopher “Chris” Dee, MD, a graduating radiation oncology resident at MSK, presented the results in a scientific session on behalf of the MSK research team.
There were 98 evaluable patients of 108 enrolled in the trial: 52 patients in the proton therapy group and 46 in the IMRT group. Among these 98 patients, 60 had parotid/salivary gland tumors, 27 had skin cancers, and 11 had tonsil cancers.
The most common histologies were squamous cell carcinoma, mucoepidermoid carcinoma, and adenoid cystic carcinoma. Five patients also received platinum-based chemotherapy.
The intent-to-treat analysis found that the rate of acute grade 2 or higher mucositis in the proton group was 7.5%, significantly lower than 22.2% in the IMRT group (p = 0.0376). Results for the as-treated analysis were similarly significant, with a rate of 7.7% of acute grade 2 or higher mucositis in the proton radiotherapy group versus 21.7% in the IMRT group (p = 0.045). Proton beam radiotherapy also had a lower incidence of acute grade 2 or higher dysgeusia (7.7% versus 33%, p=0.002).
The analysis found no significant differences between proton beam radiotherapy and IMRT for the secondary endpoints of local control, regional control, and distant metastasis-free survival. The three-year PFS rates were 92.3% for the proton therapy group and 94.1% for the IMRT group and the three-year OS rates were 97.4% and 97.6%, respectively. For the additional toxicities evaluated, there were no significant differences between groups for acute dermatitis, acute dysphagia, or late toxicities.
Patient-reported outcomes of functional and global health were higher for proton beam radiotherapy versus IMRT. More patients in the IMRT group reported mouth and throat soreness, higher skin burn sensitivity, and skin darkening that affected their quality of life.
“Taken together, this data shows that proton beam radiotherapy can achieve disease control and survival comparable to IMRT, with less toxicity and confer an improved quality of life to patients with a range of head and neck cancers,” Dr. Dee said.
“At MSK, we are proud to lead the generation of data showing proton beam radiotherapy is superior to IMRT in head and neck cancers that undergo ipsilateral radiation therapy, especially for lowering toxicities that are critical to patients,” Dr. Lee said.
Read ASTRO 2025 Abstract 241: A Phase 2 Randomized Study of Proton vs. Intensity-Modulated Radiation Therapy in the Treatment of Unilateral Head and Neck Cancer.
The study was funded by the MSK Department of Radiation Oncology Learn more about MSK clinical trials for patients with head and neck cancers.