Imagine a blood test that detects the first signs of a brain tumor when it might be treated more easily.
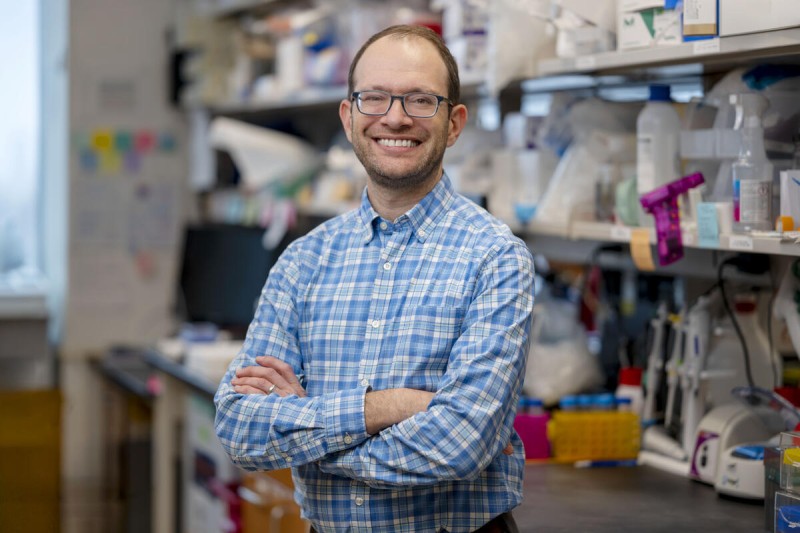
A liquid biopsy for brain cancers is now one step closer to reality. The laboratory of Memorial Sloan Kettering Cancer Center (MSK) biomedical engineer Daniel Heller, PhD, has developed an ultrasensitive diagnostic test that could potentially detect and classify different types of brain tumors with 98% accuracy. The technology combines artificial intelligence (AI) with sensors made of carbon nanotubes, tiny rod-like particles nearly 100,000 times smaller than the width of a human hair.
The approach also enabled the researchers to identify cancer-associated protein biomarkers that were previously unknown. The team published their findings in Nature Nanotechnology.
A New Kind of Liquid Biopsy That Detects Proteins
Most liquid biopsies have focused on detecting molecules such as DNA from tumor cells that have spilled into the bloodstream. But a blood test for brain tumors requires a different approach. The tight seal of the blood-brain barrier prevents most cancer cells and their genetic material from leaking into the blood.
Dr. Heller’s technology overcomes this challenge by using carbon nanotubes to look for alterations in proteins and other molecules that might change throughout the body in response to the brain tumor.
“The nanosensors detected changes in molecules in the blood, not just from the brain tumor cells, but also from the surrounding tissues and from the immune system throughout the body — the combination known as the tumor ecosystem,” says Dr. Heller, head of the Cancer Nanomedicine Laboratory at MSK.
Looking for Fluorescent Patterns To Detect and Distinguish Tumors
The carbon nanotubes are fluorescent, and the light they give off is very sensitive to minute interactions with molecules in their environment. The combined responses of all the protein-sensor interactions create a unique fluorescent pattern.
“By using machine learning, we can distinguish the fingerprint of normal cells and different cancers,” Dr. Heller says. “These sensors not only detected the presence of tumors, they also for the first time showed us which proteins are involved and where they came from — which turned out to be from all over the tumor ecosystem.”
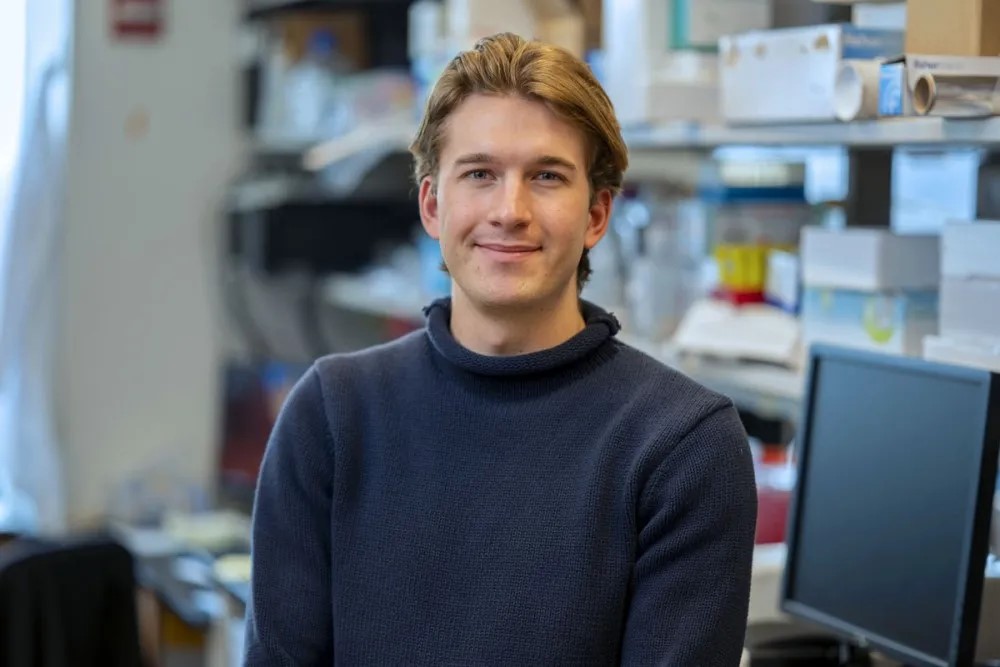
“This nanosensor platform is so sensitive because it detects signals from many different molecules that together enable ‘perception’ of the tumor, the way a nose allows you to perceive a certain scent,” says Dana Goerzen, a PhD student with the Heller Lab and the study’s first author.
“The signals not only detected the tumor, they also allowed us to tell the difference between tumor types, such as glioblastoma and meningioma,” he adds. “This is important especially when an MRI is not so clear. We could also detect indolent tumors, which are slow-growing and release fewer molecules into the bloodstream.”
Dr. Heller’s Cancer Nanotechnology Lab uses the latest cancer science and technology — focused not only on building sensors to detect the disease but also exploring new drug delivery systems to treat it. Dr. Heller is also Co-Director of the Pat and Ian Cook Doctoral Program in Cancer Engineering, a first-of-its-kind PhD program training students in cancer engineering techniques.
Dr. Heller and his team had previously demonstrated the promise of carbon nanosensors to detect ovarian cancer. The new research shows the technology can not only detect brain tumors but also distinguish the tumor types, making a tool that could potentially aid doctors in reaching a diagnosis and treatment plan while reducing the need for more invasive tests.
Using AI to Analyze Blood Samples From Brain Tumor Patients
To train the machine-learning “perception” algorithm, the researchers analyzed many blood samples from brain tumor patients.
“It’s similar to programming a self-driving car,” Dr. Heller says. “If you get millions of hours of data from a car traveling through the whole city, the algorithm will be trained better, and the car will crash less often. In our case, the technology works better with samples from more patients.”
The team collected 739 blood samples and exposed the blood to the nanosensors, which emit fluorescent signals. The researchers used machine learning to look for patterns in the signals associated with tumors.
As the blood samples were analyzed with the sensors and AI, distinct fingerprints began to take shape. Some molecules interacting with the nanosensors were common to multiple cancers, while others were associated with specific tumor types, enabling different cancer types to be distinguished.
Discovering New Cancer Markers
Dr. Heller says the study allowed them to identify proteins that previously had not been associated with cancer. Once the researchers identified patterns associated with cancer, they could look at the individual elements — the proteins — within the pattern.
“We didn’t have a hypothesis about what we would detect, but our collaborator, Dr. Alban Ordureau, was able to use mass spectrometry to determine which proteins stuck to the sensors,” Dr. Heller says. (Mass spectrometry separates the parts of a molecule based on their masses.) “It’s like we first peeked in the back of the test book to see the answer — can it detect cancer or not — and then we worked backwards to try to understand what molecules contributed to the cancer signal.”
As more samples are analyzed, the researchers will continue to refine the nanosensor approach to be more accurate at identifying cancers and to discover more biomarkers.
In the short term, the liquid biopsy could be helpful for doctors assessing people at higher risk for brain tumors, either because they have a family history or have certain symptoms. Patients might avoid an invasive biopsy.
“We hope to use this technology to develop a clinical test that could improve diagnosis, as well as to discover even more biomarkers that shed light on the diseases,” Dr. Heller says. “This collaboration between engineers, clinicians, and biologists made a technology that could prevent cancer mortality and also find new information about these deadly cancers that could help in the development of new treatments.”
Key Takeaways
- A new technology developed at MSK used carbon nanotubes and artificial intelligence to detect cancer-related proteins shed from the brain into the bloodstream.
- Early results from the testing of this new liquid biopsy showed the method could detect and classify different types of brain tumors with 98% accuracy.
- The nanotube sensors detected changes in proteins from brain cancers, cells surrounding the tumors, and the immune system.
- If validated, the test could be used to monitor people at higher risk for brain tumors and to help diagnose them earlier.
Additional Authors, Funding & Disclosures
Additional MSK authors on the study are Alban Ordureau, Mijin Kim, Margaret Ngoc Hoang, Jaina Sarris Wollowitz, and Sana Raoof.
The authors acknowledge funding from:
MSK Support Grant (P30CA008748), National Institute of Biomedical Imaging and Bioengineering (R01-EB033651), National Science Foundation CAREER Award (1752506), National Science Foundation DMREF (2323759), New York State Biodefense Commercialization Fund, Honorable Tina Brozman Foundation for Ovarian Cancer Research, and Ovarian Cancer Research Alliance, the Expect Miracles Foundation: Financial Services Against Cancer, and the Cycle for Survival’s Equinox Innovation Award in Rare Cancers. [Dr. Heller]
Canadian Institutes for Health Research Doctoral Foreign Study Award (DFD-193220) and General Atlantic Predoctoral Fellowship. [Dana Goerzen]
Sloan Kettering Institute startup funds and National Institute of General Medical Sciences (R35GM156454) [Dr. Ordureau]
Dr. Heller is a co-founder, board member, and officer with equity interest in Nine Diagnostics Inc., a co-founder with equity interest and intellectual property interests in Selectin Therapeutics Inc., and a co-founder with equity in Lime Therapeutics Inc. He is a member of the scientific advisory boards of Concarlo Therapeutics Inc., Celine Therapeutics Inc., Nanorobotics Inc., and Mediphage Bioceuticals Inc., and a consultant for Metis Therapeutics Inc.