Estrogen receptor (ER)–positive breast cancer is the most common type of the disease. About two-thirds of all breast cancers initially respond to estrogen-blocking drugs, such as tamoxifen (Nolvadex®, Soltamox®). Many people with this form of disease can be cured with a combination of surgery and other treatments. If the disease comes back, however, it’s generally widespread and resistant to hormone therapy — and therefore very difficult to treat. For these reasons, experts consider this type of breast cancer an important area of study.
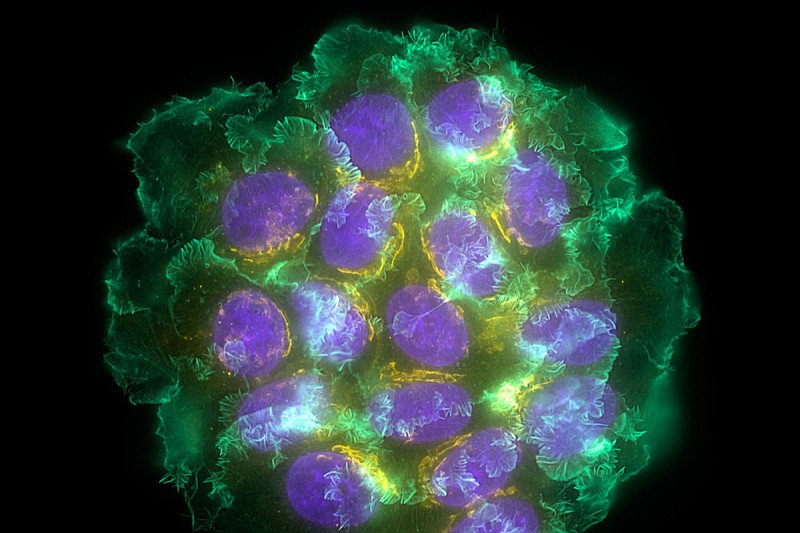
Researchers have known for a while that from the time any tumor first forms, it releases cancer cells that can travel through the bloodstream and hide out in the body. Even if the original tumor is successfully treated, those dormant cells may linger, sometimes for decades. Now investigators at Memorial Sloan Kettering have discovered a potential new way that these sleeping cancer cells wake up. The research is being reported in the Proceedings of the National Academy of Sciences.
“We know that treatments such as hormone therapy damage the mitochondria of cancer cells, which contributes to them becoming dormant,” says MSK physician-scientist Jacqueline Bromberg, the senior author of the paper. Mitochondria are the cell’s energy factories. Without them, cells are unable to grow or divide. “In this study, we’ve shown that dormant cancer cells can take up mitochondrial DNA that comes from other types of cells. They use this DNA to wake up and restore their ability to grow.”
Bubbling Up
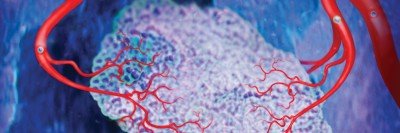
Dr. Bromberg’s lab has studied exosomes, which are tiny, bubblelike compartments, and their role in cancer for several years. In previous research, her team showed that exosomes can help cancer spread, or metastasize, by preparing organs such as the lung for the arrival of cancer cells from the breast, for example.
In the current study, her team showed for the first time that the entire DNA sequence needed to power mitochondria can be packaged inside an exosome. (Mitochondria have their own DNA separate from the cell’s nucleus.) Further, they showed that the types of cells that surround a tumor, including connective tissue and fat cells, can manufacture and release this kind of exosome.
“We have suspected for a few years now that the area around a tumor, what we call the tumor’s microenvironment, plays a huge role in the viability and growth of cancer,” says Larry Norton, Deputy Physician-in-Chief for Breast Cancer Programs at MSK and a coauthor of the paper. “This work helps us begin to understand a powerful mechanism behind this effect: the actual transfer of genetic information from the microenvironment to the cancer cells.”
Looking for Changes in the Mitochondria
In the recent set of experiments, the investigators implanted ER-positive human breast cancer cells into mice. They treated the mice with tamoxifen, and the tumors disappeared. Several months later, some of the mice developed metastatic tumors throughout their bodies. This is similar to what is seen in people with ER-positive breast cancer.
When examined, the nuclei of the cancer cells contained human DNA, as would be expected because they came from human cancer cells. The mitochondrial DNA, however, had come from the mice. This suggested that some of the genetic material inside the cancer cells had been delivered from an outside source: the tissues in the microenvironment.
Research in the animals and in the cells in the dish indicated that this mitochondrial DNA was being delivered via exosomes. It is still unknown how the exosomes package the DNA and transfer it to the cancer cells, as well as how the cancer cells take up the exosomes.
Avenues for Future Research
Dr. Bromberg says that this research has several implications for people with ER-positive breast cancer. It is still too early to know exactly if or when it may lead to new treatments.
Potentially, people who have been successfully treated for breast cancer could be regularly screened for exosomes containing mitochondrial DNA in their bloodstreams. The presence of the exosomes could indicate that dormant cancer cells may be waking up. This could allow for newly formed tumors to be detected earlier than by other methods. Additional research is focused on ways to prevent production of these exosomes.
“This is an exciting and promising area of research, but much more work is needed,” Dr. Bromberg concludes. She adds that this research may have significance for other types of cancer that are known to hide out dormant in the body, especially prostate cancer and melanoma.