-
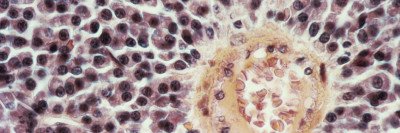
Multiple myeloma, a rare blood cancer, now has many treatment options.
- A new CAR T cell therapy targeting an antigen called GPRC5D appears to be safe and effective.
For people with multiple myeloma, prognosis has improved considerably in the past 20 years, thanks to the development of new therapies. One type of immunotherapy, called CAR T cell therapy, is showing great promise for treating this rare blood cancer.
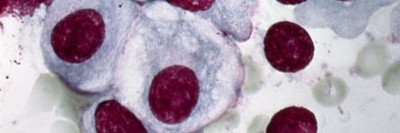
CAR T therapy genetically engineers a patient’s own immune cells to attack a protein, or antigen, on the surface of a cancer cell. Memorial Sloan Kettering Cancer Center (MSK) researchers played a pioneering role to develop CAR T cell therapy and demonstrate its safety and effectiveness in patients.
Now results from a phase 1 clinical trial show that a new CAR T cell therapy targeting an antigen called GPRC5D appears to be safe and effective. The trial, led by MSK multiple myeloma specialist Sham Mailankody, tested the CAR T therapy in 17 people with multiple myeloma for whom other treatments did not work. Overall, 71% of the patients responded to the GPRC5D-directed therapy, meaning their cancer shrank or disappeared, although some had significant side effects. Among 12 patients who received a lower dose, which had manageable side effects, the response rate was 58%.
The study is reported in the September 29, 2022, issue of The New England Journal of Medicine.
MSK Identifies New CAR T Target: GPRC5D
Most CAR T therapies for multiple myeloma have targeted an antigen called BCMA. The U.S. Food and Drug Administration (FDA) has approved two BCMA-targeted therapies in the past two years — idecabtagene vicleucel (Abecma®) and ciltacabtagene autoleucel (also known as cilta-cel or Carvytki™) — for people whose cancer didn’t respond to more conventional treatments.
But BCMA-targeted therapies don’t work for everyone.
“While BCMA-targeted therapies have shown remarkable promise, relapses are common and most patients will ultimately need additional treatment options,” Dr. Mailankody says.
In 2019, an MSK team led by physician-scientists Eric Smith and Renier Brentjens reported finding another promising multiple myeloma target — an antigen called GPRC5D. Researchers at other institutions had discovered that the GPRC5D gene was expressed in abnormally high levels in myeloma samples taken from patients. But none of those teams had been able to find the antigen on the surface of the cells.
The MSK-led team used a specialized staining technique to reveal the GPRC5D’s presence in abundance on the cell surface. In 2020, MSK launched a phase 1 clinical trial, led by Dr. Mailankody, to test GPRC5D-directed CAR T cells in people whose cancer had progressed after more conventional therapies. MSK’s Cell Therapy and Cell Engineering Facility, led by Isabelle Rivière, provided critical support by producing the CAR T cells for the trial.
“This treatment is a novel option for patients in whom other therapies didn’t work,” Dr. Mailankody says. “It’s a testament to the clinical, translational, and laboratory teams at MSK that we were able to take that preclinical lab data and open the first human study within a year — and in the middle of a pandemic. Now, just three years after the first reporting on this antigen, we have results showing the promise of a therapy targeting it.”
How the New GPRC5D CAR T Therapy Successfully Fought Robert’s Multiple Myeloma Relapse
When Robert Reinknecht retired at 58 from a career in accounting, he pictured spending leisurely days on the shore watching the waves and playing volleyball with his wife near their new house in Long Beach, New York. But in late 2014, a recurring pain in his back led to a diagnosis of multiple myeloma.
Several treatments worked for a while, but the disease kept returning. “I felt sadness and shock,” Robert says. “I thought, ‘Well, you lost.’ ”
Not long ago, Robert would have been out of options. But Dr. Mailankody enrolled him in the MSK clinical trial testing a CAR T therapy targeting BCMA. This treatment held the multiple myeloma in remission for two and a half years.
In the spring of 2021, there were signs that his disease was slowly beginning to return. Although Robert felt fine, MSK’s close monitoring of his blood and bone marrow detected the earliest stage of the disease relapsing. “I thought, ‘Oh boy, here we go again,’ ” Robert says.
Dr. Mailankody recommended Robert enroll in a second CAR T trial at MSK — this one targeting GPRC5D. In July 2021, he received a new batch of his own T cells, engineered to home in on the new target.
Having gone through CAR T treatment before made the second infusion less intimidating for Robert. At the start, he had fever and shortness of breath, but it cleared up within a week. Afterward, the only notable side effect was an odd one Dr. Mailankody had warned him about: “A few months after my infusion, my fingernails and toenails fell off,” Robert says. But they grew back.”
A year after treatment, Robert is doing very well. He continues to stay active and fully enjoy retirement.
“We go to the beach constantly and hang out with friends — I watch volleyball rather than play, but we have a great time,” he says. “I feel very lucky about everything. Thank God there are brilliant scientists and doctors who have been working on this. If it had happened to me 20 years ago, I don’t think I’d be alive.”
Now a new trial is opening at MSK, to give BCMA- and GPRC5D-targeted CAR T cell therapies together, for patients with advanced myeloma.
“We are continuing to explore possible combination approaches with this therapy as well as understand how resistance may develop,” says Dr. Mailankody. “Having an experimental treatment for patients just three years after a lab discovery is pretty remarkable — a clear sign that progress against multiple myeloma is picking up speed.”