This information explains ocular melanoma, including what it is, risk factors, and treatment.
About Ocular Melanoma
Ocular melanoma, also called uveal melanoma, is a type of eye tumor. It’s the most common eye tumor in adults. Ocular melanoma begins in the melanocyte (MEL-uh-noh-sight) cells in your eye. Ocular melanoma isn’t the same disease as cutaneous (skin) melanoma.
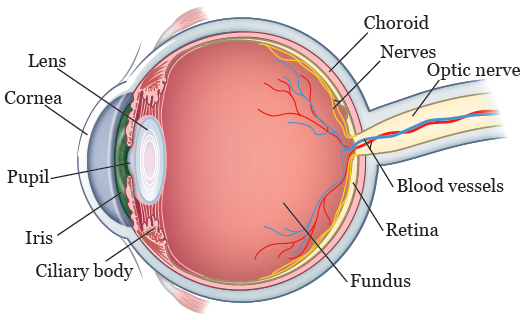
Ocular melanoma can be found in different areas of your eye (see Figure 1). Its specific name depends on where in your eye it’s found. For example:
- Iris melanoma is ocular melanoma located in your iris. Your iris is the colored area around your pupil.
- Ciliary body melanoma is ocular melanoma located in your ciliary body. Your ciliary body is the thin muscle in your eye that makes fluid and allows you to focus.
- Choroidal melanoma is ocular melanoma located in your choroid. Your choroid is the blood vessel layer within the wall of your eye, under your retina. Your retina is the layer of tissue at the back of your eyeball that senses light and helps you see.
Many people have freckles, also called nevi, in 1 or both of their eyes. Nevi aren’t ocular melanomas, but they can sometimes develop into ocular melanoma. If you have nevi, your doctor may want to keep track of their size, color, thickness, or if they’re leaking fluid. Changes in any of these things can be a sign that the nevus (freckle) is developing into ocular melanoma.
Risk factors for ocular melanoma
We don’t know the exact cause of ocular melanoma. Research studies show that unlike skin melanoma, ocular melanoma isn’t caused by common environmental factors such as sunlight, exposure to toxins, or lifestyle.
Risk factors for ocular melanoma include:
- Having blue, green, or light-colored eyes
- Being White, or having fair skin that freckles and easily burns in the sun
- Being exposed to light given off during welding
- Taking carbidopa-levodopa (Sinemet®), a medication used to treat Parkinson’s disease
Your risk for ocular melanoma also increases as you get older.
Symptoms of ocular melanoma
Most people with ocular melanoma don’t have any symptoms. For people who do have symptoms, the most common ones are:
- Blurry (not clear) vision
- Changes in vision such as blind spots or shadows, flashes of light, or seeing floating objects (floaters) in their vision
A dark spot or visible freckle on the eye can also be a sign of ocular melanoma, especially if it changes over time.
Very few people have pain.
Diagnosing ocular melanoma
To see if you have ocular melanoma, your doctor will look at the inside and outside of your eyeball. They may use special tools and imaging tests to do this.
First, your nurse will use eye drops to dilate (widen) your pupil. This makes it easier to see into your eyeball. You may feel a slight burning or stinging feeling from the eye drops that are used.
After your pupil is dilated, a technician will use special cameras and imaging tools to look at your eyeball. Examples of these cameras and tools include:
- Optical Coherence Tomography (OCT): OCT uses light to take pictures of the layers of your retina. OCT uses a bright light, but it isn’t painful.
- Ultrasound: An ultrasound uses sound waves to create an image of the inside of your eyeball. A probe (wand) covered in gel is placed on the outside of your eyeball. This gel is safe for your eye. Although you might feel some pressure from the probe or a cool sensation from the gel, ultrasound isn’t painful.
- Optos®: Optos is an advanced camera that takes pictures of your fundus (the back of your eyeball).
- Transillumination: Transillumination (tranz-ih-loo-mih-NAY-shun) uses a very bright light to show the location of tumors inside your eyeball. With transillumination, a probe is placed on the outside of your eyeball and a bright light is shined through your eyeball for several seconds. You may see bright spots for a few minutes afterward. Although you may feel some pressure from the probe on your eyeball, transillumination isn’t painful.
- Contrast or dye studies: An intravenous (IV) line is placed in your arm or hand and dye is injected. Pictures are taken to look at blood vessels and blood flow in your retina and choroid.
Your pupil will stay dilated for a few hours after your appointment. This can make reading or using a computer screen hard. It may also make you more sensitive to light than usual. Bring sunglasses to protect your eyes from light. If you usually drive to and from your appointments, bring a person who can drive you home.
Follow-up for ocular melanoma
Once a diagnosis has been made, you will have regularly scheduled eye exams with your ophthalmic oncologist (doctor who specializes in eye cancers). During these visits, your doctor may use some of the same tools and imaging tests described in the “Diagnosing Ocular Melanoma” section.
It’s very important that you go to all of these appointments so the cancer can be closely monitored. If ocular melanoma spreads, it usually spreads through the bloodstream to the liver. You and your doctor will discuss this. Your doctor may recommend having an ultrasound or MRI of your abdomen (belly) at least once each year.
Treatments for ocular melanoma
There are several ways to treat ocular melanoma. Your doctor will talk with you to decide what treatment is best for you. You may have 1 or more of the following treatments.
Observation or “watchful waiting”
If you don’t have any symptoms, or if your symptoms are manageable, you and your doctor may decide to carefully watch the tumor for a period of time without giving any other treatment. Many people choose watchful waiting until symptoms appear or change.
If you choose watchful waiting, you will have regular follow-up tests and eye exams. It’s important to go to these appointments.
Brachytherapy
Brachytherapy is a type of radiation therapy. In this type of treatment, your doctor will work with a radiation oncologist to create a small disc (plaque) that fits on your eye and delivers radiation to the tumor. The plaque will be placed on your eye by an ophthalmology (eye) surgeon during a surgery.
The plaque will stay on your eye for a few days, until the tumor gets the right amount of radiation. You will be in the hospital the whole time the plaque is in place. Because small amounts of radiation will reach the space around you, you will have a single room . No one under the age of 18 or who is pregnant can visit you.
Once the tumor has received the right amount of radiation, the plaque will be removed during another surgery and you will be able to go home. For more information, read our resource About Ocular Brachytherapy. You can search for it on our website, www.mkscc.org/pe, or you can ask your nurse.
Enucleation
Enucleation is having your eye removed during a surgery. With enucleation, tissue around your eyeball (such as your eyelid) is left in place. You may feel some discomfort after your surgery, but most people don’t feel pain. Enucleation is done in the operating room, and most people go home the same day.
Once you are healed after your surgery, you will meet with an ocularist. An ocularist is someone who makes and fits ocular prostheses (fake eyes). Your ocularist will work with you to make a fake eye that matches your other eye. They will teach you how to care for the fake eye.
Laser photocoagulation
Laser photocoagulation is therapy that uses a special type of laser to burn and destroy the tumor. Most people have laser photocoagulation after brachytherapy. The first session is usually done during the surgery to remove the plaque from your eye. After that, you’ll come back to the office for 2 more treatments.
After the first session, laser photocoagulation is done in the office while you’re awake. Before the procedure begins, you’ll get numbing drops in your eye. Your eye may feel warm during the procedure, but you won’t feel any pain.
Proton beam radiation
Proton beam radiation is another way of delivering radiation to the tumor. It can be effective for treating tumors next to the optic nerve and is like plaque radiation therapy. It also requires surgery in the operating room to place markers on the eye. This is followed by 5 weekdays of radiation therapy at the New York Proton Center (NYPC).
About genetic testing for ocular melanoma
Some studies have shown that people who have ocular melanoma and who also have a mutation in the BAP1 (BRCA associated protein 1) gene may be at higher risk for metastases (the cancer spreading).
Your doctor may recommend that you be tested for a BAP1 mutation if you have been diagnosed with ocular melanoma and you:
- Are younger than 30 years of age
- Have had another cancer in the past, especially if it was lung cancer, kidney cancer, stomach cancer, or a skin melanoma
- Have a family member who has had cancer, especially if it was lung cancer, kidney cancer, stomach cancer, or a skin melanoma
If you’re interested in genetic testing, tell your doctor or nurse. They will refer you to one of our genetic counselors.
Call your healthcare provider if you have:
- Sudden loss of your vision
- Sudden change in your vision
- Any pain
Resources
Ocular Melanoma Foundation
Has information and support for people managing ocular melanoma.
www.ocularmelanoma.org
Melanoma Research Foundation
Has information about prevention, diagnosis, and treatment of melanoma.
www.melanoma.org
National Cancer Institute (NCI)
Has information about ocular melanoma, including its causes, screening, and treatment.
www.cancer.gov/types/eye
800-4-CANCER (800-422-6237)
