This information explains brachytherapy for ocular (eye) tumors, including how to get ready and what to expect during and after your treatment.
About ocular brachytherapy
Brachytherapy is a type of radiation therapy. With brachytherapy, radioactive seeds are placed inside or close to the tumor(s). This means that the tumor gets a large amount of radiation, while nearby healthy tissue gets less radiation and is less likely to be damaged.
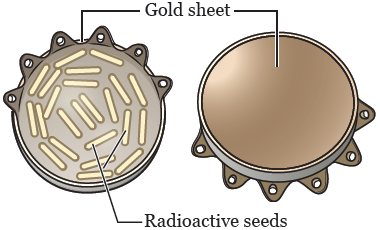
With ocular (eye) brachytherapy, a gold plaque (thin gold sheet) with radioactive seeds is placed on the surface of your eye during a surgery (see Figure 1). The gold protects other areas of your body from radiation from the seeds.
The brachytherapy is treating the whole time the plaque is on your eye. This is usually for 2 to 4 days. You will stay in the hospital and be on radioactive isolation during your brachytherapy.
To end the brachytherapy, the plaque will be removed during another surgery.
Before your plaque placement procedure
Presurgical testing (PST)
You’ll have a PST appointment before your procedure. You’ll get a reminder from your healthcare provider’s office with the appointment date, time, and location. Visit www.msk.org/parking for parking information and directions to all MSK locations.
You can eat and take your usual medicines the day of your PST appointment.
It’s helpful to bring these things to your appointment:
- A list of all the medicines you’re taking, including prescription and over-the-counter medicines, patches, and creams.
- Results of any medical tests done outside of MSK in the past year, if you have them. Examples include results from a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
You’ll meet with an advance practice provider (APP) during your PST appointment. They work closely with MSK’s anesthesiology (A-nes-THEE-zee-AH-loh-jee) staff. These are doctors with special training in using anesthesia during a procedure.
Your APP will review your medical and surgical history with you. You may have tests to plan your care, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your APP may recommend you see other healthcare providers. They’ll also talk with you about which medicine(s) to take the morning of your procedure.
For pediatric patients: pediatric pre-admission testingWithin 30 days of your procedure, you and your child will meet with their MSK pediatrician for pediatric pre-surgical testing (PPST). Your child can eat and take their usual medicines the day of their PPST appointment. During this appointment, your child’s pediatrician will review their medical and surgical history with you. Be sure to tell them about any medical problems your child has, as well as if they have have gotten anesthesia in the past. Depending on their medical and surgical history, your child may have additional tests, such as blood tests or an electrocardiogram (EKG). Their pediatrician may also recommend that they see other healthcare providers, such as a cardiologist (heart doctor). |
Radiation therapy appointment
About 1 week before your procedure, you will meet with members of your radiation oncology team. They will review the details of the procedure with you. Your radiation oncologist will determine the size of your plaque and the length of time you will need to wear it. This will be based on the measurements taken during the first appointment you had with your ophthalmologist (eye doctor).
Fill out a Health Care Proxy form
If you have not already filled out a Health Care Proxy form, we recommend you do now. If you already filled one out or have any other advance directives, bring them to your next appointment.
A health care proxy is a legal document. It says who will speak for you if you cannot communicate for yourself. This person is called your health care agent.
- To learn about health care proxies and other advance directives, read Advance Care Planning for People With Cancer and Their Loved Ones.
- To learn about being a health care agent, read How to Be a Health Care Agent.
Talk with a member of your care team if you have questions about filling out a Health Care Proxy form.
Ask about your medicines
You may need to stop taking some of your usual medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking.
We’ve included some common examples below, but there are others. Make sure your care team knows all the prescription and over-the-counter medicines you take. A prescription medicine is one you can only get with a prescription from a healthcare provider. An over-the-counter medicine is one you can buy without a prescription.
It is very important to take your medicines the right way in the days leading up to your procedure. If you don’t, we may need to reschedule your procedure.
Aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs)
Some medicines can cause bleeding. Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil for important information about stopping medicines before your procedure.
Herbal remedies and supplements
If you take herbal remedies or supplements, stop taking them 7 days before your procedure. To learn more, read Herbal Remedies and Cancer Treatment.
Blood thinners
If you take a blood thinner, ask the doctor who prescribes it for you when to stop taking it. These are some examples of blood thinners:
| aspirin | dabigatran (Pradaxa®) | rivaroxaban (Xarelto®) |
| apixaban (Eliquis®) | enoxaparin (Lovenox®) | warfarin (Coumadin®) |
| clopidogrel (Plavix®) | heparin |
There are others, so be sure your doctor knows all of the medicines you’re taking.
Medicines for diabetes
If you take insulin or other medicines for diabetes, ask the doctor who prescribes it what you should do the day before and the morning of your procedure.
1 day before your plaque placement procedure
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
For pediatric patients: Instructions for eating and drinking before your procedure
Your NP will talk with you about what your child can and cannot eat before their procedure. |
Instructions for showering
Shower using soap and water the night before or the morning of your procedure.
The day of your plaque placement procedure
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Take your medicines
If your doctor or NP told you to take certain medicines the morning of your surgery, take only those medicines with a sip of water. Depending on what medicines you take, this may be all, some, or none of your usual morning medicines.
Things to remember
- If you wear contact lenses, wear your glasses instead.
- Do not put on any lotion, cream, deodorant, makeup, powder, or perfume.
- Do not wear any metal objects. Take off all jewelry, including body piercings.
- Leave valuables, such as credit cards, jewelry, or your checkbook, at home.
Where to go
Your procedure will be at MSK’s main hospital. Its address is 1275 York Ave. (between E. 67th and E. 68th streets). Take the M elevator to the 2nd floor and check in with the Presurgical Center (PSC) concierge.
For pediatric patients: Where to goYour procedure will be at MSK’s main hospital. Its address is 1275 York Ave. (between E. 67th and E. 68th streets). It will be at one of the following locations:
Your doctor or nurse will tell you where to go for your procedure. |
After you check in, you will meet with your nurse. Tell them the dose of any medicines (including patches and creams) you took after midnight and the time you took them.
During your procedure
When it’s time for your surgery, you will either walk into the operating room or be taken in on a stretcher. A member of your operating room team will help you onto the operating bed. Compression boots will be placed on your lower legs. These gently inflate and deflate to help circulation in your legs.
Once you’re comfortable, you will get anesthesia (medicine to make you sleep) during your procedure. After you’re asleep, a breathing tube will be placed through your mouth and into your windpipe to help you breathe.
Your ophthalmologist and radiation oncologist will work together to stitch the plaque in place on your eye. Once the procedure is complete, the breathing tube will be removed and a bandage will be placed over your eye.
After your procedure
When you wake up after your surgery, you will be in the Post Anesthesia Care Unit (PACU).
You will receive oxygen through a thin tube that rests below your nose called a nasal cannula. A nurse will be monitoring your body temperature, pulse, blood pressure, and oxygen levels.
You will stay in the PACU until you’re fully awake. After you’re fully awake, you will be taken to your hospital room. You will stay in your hospital room for your ocular brachytherapy.
During your ocular brachytherapy
While the plaque is in place, your eye may feel scratchy. You may also feel like there’s something in your eye. Most people don’t feel that the plaque is painful. If you do have pain, your doctor will give you medicine to make you comfortable.
The plaque is designed so the radioactive seeds are on the inside, facing your eye, and the gold sheet is on the outside. This limits the amount of radiation that reaches the space around you. However, you’ll be on radiation precautions while the plaque is in place. For more information, read “Radiation safety precautions.”
Your medical team will visit you each day. They will remove the bandage and place a cream in your eye. The cream will help prevent infection and reduce inflammation. You may have double vision or limited vision when the bandage is removed for this exam.
Once your brachytherapy is finished, you will have another surgery to remove the plaque. The surgery will be the same as the one to place the plaque, except it will be removed instead. You may also have laser treatment during this surgery. Not everyone will have laser treatment. If you’re having laser treatment, your doctor or nurse will give you more information.
Radiation safety precautions
While your plaque is in place, there will be a small amount of radiation coming from your eye.
- Avoid being in close physical contact with other people for a long period of time. It’s fine to be in close contact with another person for a short period of time (such as a brief hug). You should stay at least 3 feet (about an arm’s length) away from other people most of the time.
- You will need to stay in a private room during your hospital stay. Pregnant people or children under age 18 will not be able to visit.
After your ocular brachytherapy
You will be able to go home the same day the plaque is removed. You will no longer need to follow radiation precautions.
You will go home with a bandage over your eye. You will also get prescriptions for pain medicine, eye drops, and eye cream(s) before you leave the hospital.
Call your doctor’s office to schedule a follow-up appointment after your treatment. Your first follow-up appointment should be 4 weeks after you finish treatment.
At home
- Keep the bandage on your eye for 2 days after your surgery.
- After you remove the bandage, start using the creams and eye drops that your doctor prescribed. Be sure to follow your doctor’s instructions.
- After you remove the bandage, you may use warm water and mild soap (such as Dove®, Basis®, or Cetaphil®) to wash your face. Rinse the skin well, and pat dry with a soft towel.
- Avoid scratching or rubbing your eye.
- Take your pain medicine as directed and as needed.
Side effects of ocular brachytherapy
You may have side effects after your brachytherapy.
Some side effects happen soon after your treatment and usually last from a few days to a few weeks. Examples include:
- Double vision or blurry vision. You can use an eye patch to make these easier to manage.
- Swelling, redness, or dryness of your eye. Your doctor will give you eye drops or cream to help manage these symptoms.
Other side effects usually happen 18 months or longer after treatment, but they may happen sooner. Examples include:
- Dryness of your eye that doesn’t go away. You can keep using lubricating eye drops or cream to help manage this.
- Cataracts (cloudiness in the lens of your eye). This happens more often if the tumor was near the front of your eye and your cornea.
- Damage to your retina (radiation retinopathy). Your retina is the layer at the back of your eyeball that senses light and helps create images. Radiation retinopathy happens more often if the tumor was near the back of your eye and your optic nerve. It usually develops slowly, months or sometimes years after radiation.
- Vision loss. Most people eventually lose vision in the area of their eye where the plaque was placed. The amount of vision loss depends on where the plaque was placed. You may notice vision loss 12 to 18 months after your treatment. You can talk with your doctor about the possibility of vision loss in your eye.
Follow-up after your treatment
After your treatment is done, it’s important to have regular follow-up appointments with your oncologists and ophthalmologists. You may need blood tests, x-rays, and scans to see how you responded to your brachytherapy.
Before your visits, write down any questions and concerns you have. Bring this and a list of all your medicines with you to your appointments.
If you’re running low on any of your medicines, tell your doctor before you run out. You can also call your doctor or nurse at any time between follow-up visits if you have any questions.
Emotional concerns
After surgery for a serious illness, you may have new and upsetting feelings. Many people say they felt weepy, sad, worried, nervous, irritable, and angry at one time or another. You may find that you can’t control some of these feelings. If this happens, it’s a good idea to seek emotional support.
The first step in coping is to talk about how you feel. Family and friends can help. Your nurse, doctor, and social worker can reassure, support, and guide you. It’s always a good idea to let your care team know how you, your family, and your friends are feeling emotionally. Many resources are available to patients and their families.
Resources
Ocular Melanoma Foundation
Has information and support for people and caregivers managing ocular melanoma.
www.ocularmelanoma.org
Retinoblastoma Information
Information about retinoblastoma from MSK’s website.
www.msk.org/pediatrics/cancer-care/types/retinoblastoma
National Eye Institute
Has information about eye health and eye diseases.
www.nei.nih.gov
Eye Cancer Network
Has information about eye cancer and related diseases.
www.eyecancer.com
When to call your healthcare provider
Call your healthcare provider if you have:
- Pain that doesn’t get better with medicine.
- Intense headaches.
- Nausea (feeling like you’re going to throw up).
- Vomiting (throwing up).
- Bleeding through the dressing.
- Yellow or green drainage.
Call your doctor right away if you have a fever of 100.4 °F (38 °C) or higher.
Contact information
If you have any questions or concerns, talk with a member of your healthcare team. You can reach them Monday through Friday from to
After , during the weekend, and on holidays, call 212-639-2000. Ask for person on call for your doctor.
