This information explains your spinal cord stimulator (SCS), including how it works and how it’s placed.
About your SCS
An SCS is a small, round device that’s used to treat pain. It’s implanted (surgically placed) under your skin in your abdomen (belly) or upper buttocks and your upper spine. The SCS works by sending electrical signals to the nerves around your spine. The electrical signals block your nerves from feeling pain.
SCSs are usually used to treat:
- Lower back pain, most often after surgery.
- Arm, chest, abdomen, or leg pain.
- Pain after shingles, including pain in your face.
- Severe (very bad) nerve pain that does not get better with other treatments.
A SCS may not be the right treatment for you if you:
- Have a pacemaker.
- Have a bleeding problem, such as a low platelet count.
- Are taking a blood thinner. This is medicine that affects the way your blood clots.
- Have a curved spine.
Talk with your doctor about other treatment options.
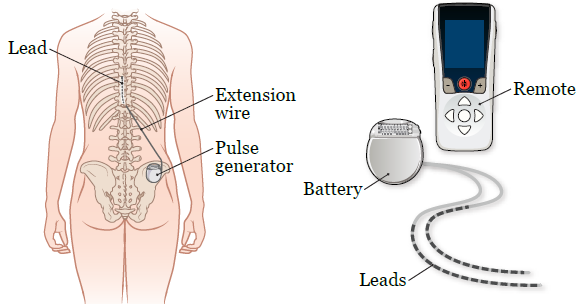
The parts of your SCS
The SCS has 3 main parts: the battery, the leads, and a wireless remote (see Figure 1).
- The battery is the round part of the device. It’s about the size of a matchbook and weighs about 2 ounces. The battery is implanted into your abdomen or upper buttocks.
- The leads are the wires coming out of the battery. You will have 1 or 2 leads. These are implanted in your upper spine.
- The remote is a handheld device that comes with your SCS. You can adjust the settings of your SCS using the remote. Your doctor will give you more information about how and when to adjust your settings.
The battery sends electrical signals through the leads to your nerves to block them from feeling pain.
SCS screening test
Before you get an SCS, you will have a screening test to see if it will help with your pain. For your screening test, you will have a lead implanted into your spine. The other end of the lead will be attached to a temporary SCS battery. It will be taped to the skin above your waist.
You will also get a remote to adjust the settings of your SCS. You will leave the hospital with the SCS in place.
You will wear the temporary SCS for about 7 to 10 days. You will have a follow-up appointment with your doctor. They will remove the SCS at your appointment. They will also talk with you about a permanent SCS and if it will help you manage your pain.
Your doctor will give you more information about your SCS screening test. They will tell you what to expect and how to get ready for it.
About your SCS placement
If you and your doctor decide this treatment is right for you, you will have surgery to implant your SCS. Your nurse will give you more information about your surgery and tell you how to get ready.
You will have to wait about 10 days after your temporary SCS is removed to have your surgery. This will give your body time to heal after having your temporary SCS removed.
Most health insurers, including Medicare, cover the cost of the SCS screening test and placement. Call your insurer and ask if you will be covered.
Your health insurer may also want you to have psychological testing before it approves the permanent SCS. Call them for more information.
What to expect during surgery
You will get anesthesia (medicine to make you sleep) before your surgery starts.
Once you’re asleep, your doctor will make a small incision (surgical cut) in your abdomen or upper buttocks to place the battery. The battery will look like a small bulge under your skin.
Your doctor will use fluoroscopy (floor-OS-koh-pee) to find the exact area to place the leads. This is a type of X-ray procedure.
Your doctor will place the leads around your spine using 2 small needles. Then they will connect the leads to the battery. They will close your incision with staples or sutures (stitches).
Your surgery will take 1 to 3 hours.
After your surgery, you will be taken to the recovery room. Your doctor will program your SCS to give you pain relief. Instead of pain, you may feel tingling. Your nurse will teach you how to adjust the strength and settings of your SCS using the remote.
You will have your SCS in place for as long as you need it to help you manage your pain.
Your SCS may set off metal detectors. You will get an identification (ID) card that says you have an implanted device. You must carry this card with you at all times while you have your SCS in place. You will get this card in the hospital or it will be sent to you a few weeks after your surgery.
What to expect after surgery
After your surgery, your incisions may be sore. You will be given a prescription for pain medicine before you leave the hospital. Talk with your healthcare provider about possible side effects.
They will also tell you when you can switch to over-the-counter pain medicine. This is medicine you buy without a prescription.
- Do not lift anything heavier than 10 pounds (4.5 kilograms).
- Do not bend over, such as to pick something up from the ground.
- Do not twist your body, such as to crack your back.
- Do not put your body in very hot or cold temperatures. This includes a sauna, hot tub, or ice bath.
Follow-up appointments
- You will have a follow-up appointment with your doctor 1 to 2 weeks after your surgery. Your doctor will take out your sutures during this appointment.
- You will have a follow-up appointment with your pain doctor 1 to 2 months after your surgery. They will check if your SCS is helping you with your pain.
- You will also have follow-up appointments every 1 to 3 months. Your doctor will adjust the settings of your SCS to better treat your pain.
Contact information
If you have any questions or concerns, call the Anesthesia Pain Service at 212-639-6851. You can reach a staff member Monday through Friday from to After , during the weekend, or on holidays, call 646-699-8322 and ask for the anesthesia pain person on call.