This information explains Aquablation therapy and how to get ready for it. This is a treatment for benign prostatic hyperplasia (beh-NINE prah-STA-tik HY-per-PLAY-zhuh), also called BPH. This resource also explains parts of the male reproductive system.
About your prostate
-
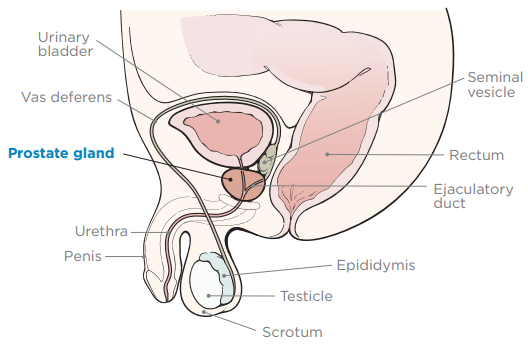
Your prostate is a small, firm gland about the size of a walnut. It’s in front of your rectum, below your bladder (see Figure 1). Your prostate works with other glands in your body to make semen.
- Your urethra is a tube that carries urine (pee) from your bladder, through your penis, and out of your body.
- Your seminal vesicles are small glands near your prostate that make the fluid in semen.
About BPH
BPH is when your prostate is enlarged (bigger than normal). With BPH, your prostate presses down on your urethra. This makes it hard to urinate (pee). If you don’t empty your bladder for long periods of time, you may get:
- A urinary tract infection (UTI).
- Bladder stones.
- Bladder diverticulum (DY-ver-TIH-kyoo-lum). This is when your bladder wall stretches and creates pockets that collect urine.
- Kidney damage from urine that backs up to the kidneys. This happens when the urethra is blocked.
About Aquablation
Aquablation is used to treat BPH when medicine does not work. During Aquablation, your surgeon will use ultrasound, robotics, and a water jet to remove part of the prostate tissue. This makes it easier to urinate and provides long-lasting relief.
After the surgery is finished, your surgeon will cauterize (KAW-teh-RIZE) parts of the prostate that are more likely to bleed. This process seals off blood vessels to stop bleeding. They will use a tool with an electric current to burn or dissolve the tissue.
What to do before your Aquablation
Getting ready for your surgery
You and your care team will work together to get ready for your surgery. Help us keep you safe by telling us if any of these things apply to you, even if you’re not sure.
You may need to follow special instructions before surgery based on the medicines and supplements you take. If you do not follow those instructions, your surgery may be delayed or canceled.
-
I take any prescription medicines. A prescription medicine is one you can only get with a prescription from a healthcare provider. Examples include:
- Medicines you swallow.
- Medicines you take as an injection (shot).
- Medicines you inhale (breathe in).
- Medicines you put on your skin as a patch or cream.
- I take any over-the-counter medicines, including patches and creams. An over-the-counter medicine is one you can buy without a prescription.
- I take any dietary supplements, such as herbs, vitamins, minerals, or natural or home remedies.
- I have a pacemaker, automatic implantable cardioverter-defibrillator (AICD), or other heart device.
- I have had a problem with anesthesia (A-nes-THEE-zhuh) in the past. Anesthesia is medicine to make you sleep during a surgery or procedure.
- I’m allergic to certain medicines or materials, including latex.
- I’m not willing to receive a blood transfusion.
- I use recreational drugs, such as marijuana.
Presurgical testing (PST)
You’ll have a PST appointment before your surgery. You’ll get a reminder from your surgeon’s office with the appointment date, time, and location. Visit www.msk.org/parking for parking information and directions to all MSK locations.
You can eat and take your usual medicines the day of your PST appointment.
It’s helpful to bring these things to your appointment:
- A list of all the medicines you’re taking, including prescription and over-the-counter medicines, patches, and creams.
- Results of any medical tests done outside of MSK in the past year, if you have them. Examples include results from a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
You’ll meet with an advance practice provider (APP) during your PST appointment. They work closely with MSK’s anesthesiology (A-nes-THEE-zee-AH-loh-jee) staff. These are doctors with special training in using anesthesia during a surgery or procedure.
Your APP will review your medical and surgical history with you. You may have tests to plan your care, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your APP may recommend you see other healthcare providers. They’ll also talk with you about which medicine(s) to take the morning of your surgery.
What to do the day before your Aquablation
Your surgeon may ask you to use a saline enema (such as a Fleet® saline enema) the night before your procedure.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
What to do the day of your Aquablation
Your surgeon may ask you to use a Saline Fleet® Enema the morning of your procedure.
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Things to remember
- Take only the medicine your doctor told you to take the morning of your procedure. Take them with a few sips of water.
- Do not use body creams, lotions, or petroleum jelly (Vaseline®). You can use deodorant and facial moisturizers.
- Do not wear eye makeup.
- Wear loose-fitting, comfortable clothes.
- Remove any jewelry, including body piercings.
- Leave any valuables at home if you do not need them.
- If you wear contact lenses, wear your glasses instead, if you can. If you do not have glasses, bring a case for your contacts.
What to bring with you
- Medicine for breathing problems, if you take them. This includes inhalers and medicine for your chest.
- If you wear a continuous glucose monitor (CGM), bring an extra one with you.
- A case for your glasses or contacts, if you wear them.
- Denture glue, if you wear dentures.
- Your Health Care Proxy form, if you filled one out.
- Your CPAP or BiPAP machine, if you use one. If you cannot bring yours with you, we will give you one to use while you’re in the hospital.
Where to go
Your surgery will be done at:
The Presurgical Center at Memorial Hospital on the 2nd floor
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
When you get to the hospital, take the B elevator to the 2nd floor. Check in at the desk in the Pre-Surgical Center (PSC) waiting area.
What to expect when you arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having a procedure on the same day.
When it’s time to change, you’ll get a hospital gown, robe, surgical head covering, and nonskid socks to wear.
Meet with a nurse
You’ll meet with a nurse before surgery. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicines, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist (A-nes-THEE-zee-AH-loh-jist) will do it in the operating room.
Meet with an anesthesiologist
You’ll also meet with an anesthesiologist before surgery. They will:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your surgery.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Going into the operating room
You’ll either walk into the operating room or a staff member will bring you there on a stretcher. A member of the operating room team will help you onto the operating bed. You’ll lie on your back during your surgery.
Inside the operating room
Once you’re comfortable, an anesthesiologist will give you anesthesia to make you sleep. Once you’re asleep, your surgeon will start your surgery.
What to do after your Aquablation
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your surgery. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
You’ll stay in the PACU overnight. Tell your nurse if you have any pain or discomfort. They will give you acetaminophen (Tylenol®) to help.
You will have a urinary (Foley) catheter (thin, flexible tube) in your urethra going into your bladder. This tube drains urine from your bladder so your care team can keep track of how much urine you’re making. Your care team may also use it to flush (put fluid into) your bladder. This can help lower the risk of blood clots forming.
Your nurse may remove the catheter before you’re discharged from (leave) the hospital. They may leave it in if you’re having trouble emptying your bladder when it’s time for you to be discharged. If they do, you’ll have a follow-up appointment in a few days so your nurse can take it out.
What to expect at home
Your healthcare provider will give you an antibiotic to take when you go home. Take all the pills as prescribed.
You may feel discomfort or pain in your pelvic area (the area between your stomach and legs). Drinking liquids will help. You can also take acetaminophen. If the discomfort does not get better after you take acetaminophen, contact your healthcare provider’s office.
You might see tiny pieces of prostate tissue and tiny blood clots floating in your urine. This is normal. This gets better by drinking more liquids. Try to drink 6 to 8 (8-ounce) glasses of water every day.
For 2 weeks after your surgery, do not do any strenuous activities, such as jogging or playing tennis. Do not lift anything heavier than 10 pounds (4.5 kilograms). After 2 weeks, if your urine is yellow with no blood, you can go back to doing your usual activities.
You may need to urinate more often or more urgently than you did before your surgery. This gets better over time.
Some people become incontinent after surgery. This is when you cannot control your urination (pee). This is rare and will depend on how your bladder was working before your surgery. If you become incontinent, this often gets better after a few weeks.
If you’re still incontinent a few weeks after your surgery, tell your surgeon. They may order tests to see if anything can be done to make it better.
Call to make an appointment to see your surgeon 2 to 3 months after your surgery.
When to call your healthcare provider
Call your healthcare provider if you:
- Have a fever of 101 °F (38.3 °C) or higher.
- Have pain that doesn’t get better even after taking pain medicine.
- Cannot urinate.
- Have bright red bleeding in your urine that doesn’t stop.
- Have any unexpected problems.
- Have any questions or concerns.
Contact information
If you have questions or concerns, contact your healthcare provider. A member of your care team will answer Monday through Friday from 9 a.m. to 5 p.m. Outside those hours, you can leave a message or talk with another MSK provider. There is always a doctor or nurse on call.
If you’re not sure how to reach your healthcare provider, call 212-639-2000.