This information will help you get ready for your inferior vena cava (in-FEER-ee-er VEE-nuh KAY-vuh) filter placement at MSK.
About your inferior vena cava (IVC) filter
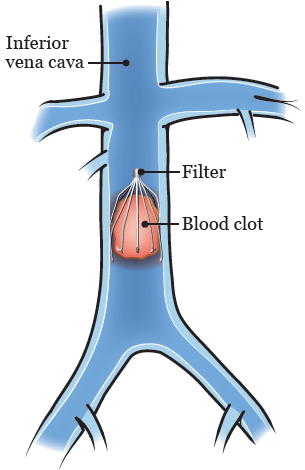
The inferior vena cava is the largest vein in your body. It carries blood from your lower body to your heart and lungs.
A blood clot in a vein below your heart blocks your normal blood flow. This may cause swelling, redness, and pain in the area. Blood clots are treated with blood thinners but some people may not be able to get this treatment. In those cases, an inferior vena cava (IVC) filter may be placed.
An IVC filter is a small device that is placed in your inferior vena cava. It traps blood clots and stops them from moving through your blood into your lungs (see Figure 1).
Your IVC filter will be placed by your interventional radiologist (also called an IR doctor). This is a doctor who has special training in doing image-guided procedures. They will place the IVC filter into your inferior vena cava through a vein in your neck or groin. Your groin is the area between your belly and thigh. Your doctor will position the IVC filter in the vein using fluoroscopy (real-time X-rays).
Some people have an IVC filter placed because they have blood clots or have a history of blood clots. Others have an IVC filter placed to get them ready for a surgery. The filter will help stop blood clots from traveling to their lungs during and after the surgery.
What to do before your procedure
Ask about your medicines
You may need to stop taking some of your usual medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking.
We’ve included some common examples below, but there are others. Make sure your care team knows all the prescription and over-the-counter medicines you take. A prescription medicine is one you can only get with a prescription from a healthcare provider. An over-the-counter medicine is one you can buy without a prescription.
It is very important to take your medicines the right way in the days leading up to your procedure. If you don’t, we may need to reschedule your procedure.
Anticoagulants (blood thinners)
A blood thinner is a medicine that changes the way your blood clots. Blood thinners are often prescribed to help prevent a heart attack, stroke, or other problems caused by blood clots.
If you take a blood thinner, ask the healthcare provider doing your procedure what to do before your procedure. They may tell you to stop taking the medicine a certain number of days before your procedure. This will depend on the type of procedure you’re having and the reason you’re taking a blood thinner.
We’ve listed some examples of common blood thinners below. There are others, so be sure your care team knows all the medicines you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Other medicines and supplements can change how your blood clots. Examples include vitamin E, fish oil, and nonsteroidal anti-inflammatory drugs (NSAIDs). Ibuprofen (Advil®, Motrin®) and naproxen (Aleve®) are examples of NSAIDs, but there are many others.
Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil. It will help you know which medicines and supplements you may need to avoid before your procedure.
Diabetes medicines
If you take insulin or other diabetes medicines, talk with the healthcare provider doing your procedure and the healthcare provider who prescribes it. Ask them what to do before your procedure. You may need to stop taking it or take a different dose (amount) than usual. You may also need to follow different eating and drinking instructions before your procedure. Follow your healthcare provider’s instructions.
Your care team will check your blood sugar levels during your procedure.
Weight loss medicines
If you take medicine for weight loss (such as a GLP-1 medicine), talk with the healthcare provider doing your procedure. Ask them what to do before your procedure. You may need to stop taking it, follow different eating and drinking instructions before your procedure, or both. Follow your healthcare provider’s instructions.
We’ve listed some examples of medicines that cause weight loss below. There are others, so be sure your care team knows all the medicines you take. Some of these are meant to be used to help manage diabetes but are sometimes prescribed just for weight loss.
|
|
Diuretics (water pills)
A diuretic is a medicine that helps control fluid buildup in your body. Diuretics are often prescribed to help treat hypertension (high blood pressure) or edema (swelling). They can also be prescribed to help treat certain heart or kidney problems.
If you take a diuretic, ask the healthcare provider doing your procedure what to do before your procedure. You may need to stop taking it the day of your procedure.
We’ve listed some examples of common diuretics below. There are others, so be sure your care team knows all the medicines you take.
|
|
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 1 day (24 hours) before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
Reactions to contrast dye
Contrast is a special dye that makes it easier for your doctor to see differences in your internal organs. Internal organs are the organs inside of your body. This procedure is usually done with contrast. The dye will be injected into a vein in your neck or groin.
Some people can have an allergic reaction to contrast. Most reactions are mild, such as hives. Some people can have very rare but more serious reactions, such as anaphylaxis (A-nuh-fih-LAK-sis). This is a bad allergic reaction that can cause hypotension (a sudden drop in blood pressure) or trouble breathing. Anaphylaxis is treated with an epinephrine (eh-pih-NEH-frin) autoinjector, commonly known as an EpiPen®. This is an injection (shot) of epinephrine (adrenaline) into a muscle.
If you’ve had a reaction to contrast in the past, tell your healthcare provider. You may need to take medicine before your procedure to help with the allergy.
If you’re breastfeeding, you may choose to continue after your procedure with contrast. If you have questions about contrast and breastfeeding, talk with your care team. They will arrange for a healthcare provider from the lactation team to contact you.
Take devices off your skin
You may wear certain devices on your skin. Before your scan or procedure, some device makers recommend you take off your:
- Continuous glucose monitor (CGM)
- Insulin pump
Talk with your healthcare provider about scheduling your appointment closer to the date you need to change your device. Make sure you have an extra device with you to put on after your scan or procedure.
You may not be sure how to manage your glucose while your device is off. If so, before your appointment, talk with the healthcare provider who manages your diabetes care.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Tell us if you’re sick
If you get sick (including having a fever, cold, sore throat, or flu) before your procedure, call your IR doctor. You can reach them Monday through Friday from to
After , during the weekend, and on holidays, call 212-639-2000. Ask for the Interventional Radiology fellow on call.
Note the time of your appointment
A staff member will call you 1 to 2 business days before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Thursday or Friday before. They’ll tell you what time to get to the hospital for your procedure. They will also remind you where to go.
If you don’t get a call by noon (12 p.m.) on the business day before your procedure, call 646-677-7001. If you need to cancel your procedure for any reason, call the healthcare provider who scheduled it for you.
What to do the day before your procedure
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
Medicine to prevent allergy to contrast dye
Your doctor may have told you to take medicine to prevent an allergy to contrast. If they did, take your first dose 13 hours before your arrival time.
What to do the day of your procedure
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Things to remember
- Follow your healthcare provider’s instructions for taking your medicines the morning of your procedure. It’s OK to take them with a few sips of water.
- If you’re taking pain medicine, take it before your procedure with a few sips of water. You can take acetaminophen (Tylenol®). Do not take any NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®).
- Do not put on body cream, lotion, or petroleum jelly (Vaseline®). You can use deodorant and facial moisturizers. Do not wear eye makeup.
- Do not wear any metal objects. Take off all jewelry, including body piercings. The tools used during your procedure can cause burns if they touch metal.
- Leave valuable items at home.
- If you wear contact lenses, wear your eyeglasses instead, if you can. If you do not have eyeglasses, bring a case for your contacts.
- Wear something comfortable and loose-fitting.
- When it’s time for your procedure, you must remove any hearing aids, dentures, prosthetic devices, wigs, and religious articles.
What to bring
- A list of all the medicines you take at home, including prescription and over-the-counter medicines, patches, and creams.
- Medicines for breathing problems (such as your inhaler), medicines for chest pain, or both.
- Your cell phone and charger.
- Only the money you may want for small purchases, such as a newspaper.
- A case for your personal items, if you have any. Eyeglasses or contacts, hearing aids, dentures, prosthetic devices, wigs, and religious articles are examples of personal items.
- Your Health Care Proxy form and other advance directives, if you filled them out.
- Your breathing device for sleep apnea (such as your CPAP machine), if you use one. If you cannot bring it, we will give you one to use while you’re in the hospital.
What to expect when you arrive
Many doctors, nurses, and other staff members will ask you to say and spell your name and date of birth. This is for your safety. People with the same or similar names may be having procedures on the same day.
Once you’re brought to the presurgical area, you’ll get a hospital gown and nonskid socks to wear. You’ll take off your eyeglasses, hearing aids, dentures, prosthetic devices, wig, and religious articles.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicines, patches, and creams.
Your nurse will place an IV line into a vein in your arm or hand, unless you already have:
- A central venous catheter (CVC) or any other type of CVC.
- A peripherally inserted central catheter (PICC).
- An implanted port (also called a mediport or Port-A-Cath).
Before your procedure, your care team will talk with you about the kind of anesthesia you’ll get. It will be given through the IV line, CVC, PICC line, or implanted port. You may also get fluids through the same line before your procedure.
Meet with a doctor
Before your procedure, you will meet the IR doctor who will place the IVC filter. They will explain the procedure to you and answer your questions. You’ll be asked to sign a consent form, which says you agree to the procedure and understand the risks.
During your procedure
When it’s time for your procedure, you’ll be brought into the procedure room and helped onto the table. You’ll lie flat on your back.
You’ll be attached to equipment to monitor (keep track of) your heart rate, breathing, and blood pressure. You’ll also get oxygen through a thin tube that rests below your nose.
Then, you’ll get sedation. This is a kind of anesthesia that will make you sleepy and relaxed.
A member of your care team will clean the skin in the area where your doctor will be working. This area is called the insertion site. The insertion site will be either your neck or groin. They will shave the area if needed and cover it with sterile (clean) drapes.
You’ll get an injection (shot) of a local anesthetic to numb the insertion site. Then, your doctor will make a small incision (surgical cut) into the site. They will insert a catheter through the incision and into a vein. There will be a closed IVC filter attached to the tip of the catheter.
Your doctor will use fluoroscopy (X-ray pictures) to guide the catheter through the vein to your inferior vena cava. The X-ray pictures will help them see where to safely place the IVC filter. Your doctor will also give you contrast dye through the catheter. The dye will help them see your inferior vena cava clearly in the pictures.
The fluoroscopy will help put catheter into place. Once it’s in the right position, your doctor will release the IVC filter from the tip of the catheter. It will expand (open up) to fit in your inferior vena cava and will stay in place there.
When the procedure is done, your doctor will take out the catheter. The site will be cleaned and covered with a dressing (bandage).
The procedure will take about 1 hour.
After your procedure
In the hospital
After your procedure, you’ll be brought to the Post-Anesthesia Care Unit (PACU). If you’re an inpatient (staying in the hospital), you’ll be brought back to your hospital room.
Your nurse will continue to monitor your heart rate, breathing, and blood pressure. They will explain your discharge instructions to you and your caregiver before you go home. They’ll also give you a wallet card with information about your IVC filter to keep with you.
Wearing a seatbelt may put pressure on your incision. You may want to place a small pillow or folded towel between the seatbelt strap and your body. This will help reduce pressure on your incision when you’re traveling home.
At home
Caring for yourself
- Leave the bandage on the insertion site for 24 hours (1 day). After 24 hours, you can take it off. Place a new bandage (Band Aid®) over the site if there is any drainage.
-
You can shower 24 hours after your procedure. Shower with your bandage in place. Gently wash around the insertion site with soap and water. Pat it dry with a clean towel.
- Change your bandage right after your shower. Place a new bandage (Band Aid®) over the insertion site. Never leave a wet bandage on. A wet bandage can irritate your skin and make it sore.
- Your insertion site must not be submerged (kept under water). Do not swim, sit in a hot tub, or take a bath until the site is healed.
- Your incision may feel sore. This should get better within 1 or 2 days. You can take over-the-counter pain medicine, such as acetaminophen (Tylenol®) or ibuprofen (Advil®), if you need it.
Activities
-
For the first few days after your procedure, avoid certain activities such as:
- Exercises that include stretching.
- Bending.
- Lifting or carrying anything heavier than 10 pounds (4.5 kilograms). This includes pets and children.
- You can still have a magnetic resonance imaging (MRI) procedure while you have an IVC filter. Make sure to tell the person doing your MRI that you have an IVC filter. Show them the wallet card your nurse gave to you. Do this every time before you have an MRI to make sure it’s safe.
- While you have an IVC filter, it’s safe to go through airport or security stations. It will not set off metal detectors.
Taking out your IVC filter
Your doctor will decide how long you will need the IVC filter and if it can be taken out. If it can, you will have another procedure to take it out. An IVC filter is often taken out 1 to 3 months after it was placed.
Not everyone can have their IVC filter taken out. Talk with you care team to see if taking out your IVC filter is right for you.
When to call your healthcare provider
Call your healthcare provider if you have:
- A fever of 100.4° F (38° C) or higher.
- Pain around your insertion site that does not get better, even after taking medicine to help.
- Drainage around your incision site.
- Redness and swelling around your insertion site.