This information will help you understand what patient-controlled analgesia (PCA) is and how to use your PCA pump.
About PCA
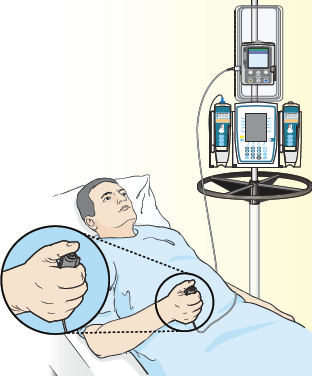
PCA helps you control your pain by letting you give yourself pain medication. It uses a computerized pump to send pain medication into your vein (called an IV PCA) or into your epidural space (epidural PCA), which is near your spine (see Figure 1). Whether you have an IV PCA or an epidural PCA depends on what you and your care team decide is right for you.
PCA is not right for everyone. Some people may not be able to use a PCA pump. Before you get a PCA pump, tell your care team if you have weakness in your hands or think you may have trouble pushing the PCA button. You should also tell your care team if you have sleep apnea. This may affect the way we prescribe your medication.
Using the PCA pump
Press the button attached to the pump when you have pain to give yourself pain medication (see Figure 1). The pump will send a safe dose of the medication your care team prescribed.
Only you should push the PCA button. Family and friends should never push the button.
The pump can be programmed to give you medication in 2 ways:
- As needed. You get your pain medication only when you press the button. It will not let you get more medication than prescribed. The pump is set to allow only a certain number of doses per hour.
- Continuous. You get your pain medication at a constant rate all the time. This can be combined with the “as needed” way. This lets you take extra doses safely if you’re having pain.
Tell your care team if the PCA is not helping with your pain. You should also tell your care team if your pain changes, gets worse, feels different than before, or if you feel pain in a new place. They may change the medication to one that may work better for you.
Side effects
Pain medication you get through a PCA can have side effects. Tell your healthcare provider if you have any of these problems:
- Constipation (having fewer bowel movements than usual)
- Nausea (feeling like you’re going to throw up)
- Vomiting (throwing up)
- Dry mouth
- Itching
- Changes in your vision, such as seeing things that aren’t there
- Drowsiness, dizziness, or confusion
- Weakness, numbness, or tingling in your arms or legs
- Trouble urinating (peeing)
- Any other side effects or problems
Your care team may change your dose or give you a different medication with fewer side effects.