This information will help you get ready for radiation therapy to your pelvis at MSK. It explains what to expect. It also explains how to care for yourself before, during, and after your radiation therapy.
This information is general. Your radiation therapy team will design a treatment and care plan just for you. Because of that, some parts of your treatment may be different than what’s described here. Your radiation therapy team will talk with you about what to expect.
About radiation therapy
Radiation therapy uses high-energy radiation to treat cancer. It works by damaging the cancer cells and making it hard for them to multiply. Your body can then naturally get rid of the damaged cancer cells. Radiation therapy also affects normal cells, but they can fix themselves in a way cancer cells can’t.
You’ll have a treatment planning procedure called a simulation before your first radiation treatment. During your simulation, your radiation therapists will take imaging scans and mark your skin with little tattoo dots. This is done to:
- Map your treatment site.
- Make sure you get the right dose (amount) of radiation.
- Limit the amount of radiation that gets to your nearby healthy tissues.
During your radiation treatments, a machine will aim beams of radiation directly to the tumor. The beams will pass through your body and damage cancer cells in their path. You will not see or feel the radiation.
Radiation therapy takes time to work. It takes days or weeks of treatment before cancer cells start to die. They keep dying for weeks or months after radiation therapy.
Radiation therapy and fertility
You must use contraception (birth control) during your radiation therapy if you’re sexually active and you or your partner could get pregnant. You should not conceive a child during your radiation therapy and for 1 to 2 years after you finish radiation therapy. To learn more, read the “Sexual and reproductive health” section of this resource.
If you want to have children after your radiation therapy, talk with your doctor before you start your radiation therapy.
Your role on your radiation therapy team
Your radiation therapy care team will work together to care for you. You’re a part of that team, and your role includes:
- Getting to your appointments on time.
- Asking questions and talking about your concerns.
- Telling us when you have side effects.
- Telling us if you’re in pain.
-
Caring for yourself at home by:
- Quitting smoking if you smoke. MSK has specialists who can help. To learn more about our Tobacco Treatment Program, call 212-610-0507. You can also ask your nurse about the program.
- Caring for your skin based on our instructions.
- Drinking liquids based on our instructions.
- Eating or avoiding the foods and drinks we suggest.
- Staying around the same weight.
What happens before radiation therapy to your pelvis
Vaginal dilator
If you have a vagina, your doctor may recommend using a vaginal dilator during your simulation and treatments. They will talk with you about this before your simulation appointment. To learn more, read Instructions for Using a Vaginal Dilator During Radiation Simulation and Treatment.
Simulation appointment
Your simulation will take 1 hour or longer. It may be shorter or longer based on your specific treatment plan.
Positron emission tomography-computed tomography (PET-CT) scan
Some people have a PET-CT scan during their simulation. If you are, your nurse will give you detailed instructions for getting ready for the scan.
Sometimes, PET-CT scans use intravenous (IV) contrast. IV contrast is a dye that’s put into your bloodstream to make the images clearer. Some people are allergic to IV contrast. If you are, your nurse will tell you what to do.
If you’re having a PET-CT scan, do not eat or drink anything except water for 6 hours before your appointment time. This includes gum, hard candy, cough drops, and mints. If you have had anything except water, we may need to reschedule your PET-CT scan.
Medicines to take
You’ll be lying still in one position during your simulation. If you think you’ll be uncomfortable, take an over-the-counter pain medicine or your usual pain medication 1 hour before your simulation. Talk with your healthcare provider ahead of time.
If you think you may get anxious during your simulation, talk with your healthcare provider ahead of time. They may suggest medicines to help.
What to eat and drink
Most people can eat and drink like usual before their simulation. Your healthcare provider will tell you if you need to follow special instructions for eating or drinking before your simulation.
What to wear
Wear comfortable clothes that are easy to take off. You will need to change into a hospital gown.
Take devices off your skin
You may wear certain devices on your skin. Before your simulation or treatment, some device makers recommend you take off your:
- Continuous glucose monitor (CGM)
- Insulin pump
If you use one of these, ask your radiation oncologist if you need to take it off. If you do, make sure to bring an extra device to put on after your simulation or treatment.
You may not be sure how to manage your glucose while your device is off. If so, before your appointment, talk with the healthcare provider who manages your diabetes care.
What to expect when you arrive
A member of your radiation therapy team will check you in when you arrive. They’ll give you an identification (ID) wristband with your name and date of birth. During your appointment, many staff members will check your ID wristband and ask you to say and spell your name and date of birth. This is for your safety. People with the same or a similar name may be getting care on the same day.
Your radiation therapists will review what to expect during the simulation. If you haven’t already signed a consent form, they will go over the form with you. They will answer any questions you have and ask for your signature.
When it’s time for your simulation, you’ll change into a hospital gown. Keep your shoes on.
Getting contrast
You may get contrast before your simulation. Contrast is a liquid that makes your small intestine easier to see on imaging scans. It can also be used to show your bladder, rectum, and vagina (if you have one).
If you need contrast, you’ll get it in 1 or more of these ways:
- Orally, as a liquid you swallow.
- Intravenously (IV), as a liquid put into your vein, if you’re not allergic.
- Through your rectum, bladder, or vagina. Your care team will put a soft rubber catheter (thin, flexible tube) into your rectum, bladder, or vagina. You will have a cloth under you to absorb any liquid that may spill out.
If you’re getting oral contrast, you’ll drink it before you go to the simulation room. If you’re getting contrast another way, you’ll get it in the simulation room.
What to expect during your simulation
Your radiation therapists will help you onto the simulation table. The table will have a sheet on it, but it’s hard and doesn’t have a cushion. If you haven’t taken pain medicine and think you may need it, tell your radiation therapists before your simulation starts.
Your radiation therapists will help you get into the right position for your simulation. You will lie on your stomach or back. Your radiation therapists may place a temporary marker near your anus. They’ll take it off at the end of your simulation. If your doctor ordered a vaginal dilator for you, follow your radiation therapists’ instructions for using it during your simulation.
Your simulation will take about 1 to 2 hours but can be shorter or longer depending on your specific treatment plan. Your radiation therapists can play music for you to help pass the time.
Do not move once your simulation starts. It’s important that you stay in the same position. If you feel uncomfortable or need help, tell your radiation therapists.
Imaging scans and positioning
Throughout your simulation, your radiation therapists will use computed tomography (CT) scans to check and adjust your position. These scans are used only to plan your treatments. They are not used for diagnosis or to find tumors.
You’ll feel the simulation table move into and out of the scanner and hear the machine turn on and off. Even if it seems loud, your radiation therapists will be able to hear you if you need to speak with them. They will walk in and out of the room during the scans, but the room has a microphone, speaker, and camera. There will always be someone who can see and hear you.
Your radiation therapist will turn the lights in the room on and off during your simulation. You will see red or green laser lights on each wall. Your radiation therapists use them to help position you on the table.
Immobilization device
Your radiation therapists may make you an immobilization device to help you stay in the same exact position for all your treatments. This may be a cushion (see Figure 1) or a mold (see Figure 2).
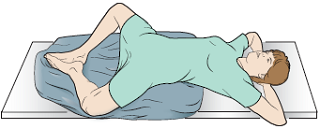

If you have an immobilization device, you’ll use it during your simulation and all your treatments. It may be attached to the simulation or treatment table, depending on your position. This helps make sure you’re in the correct position during each treatment.
Skin markings and tattoos
Your radiation therapists will use a felt marker to draw on your skin in the treatment area. Once they’re sure you’re in the right position, they will make tattoos using a sterile needle and a drop of ink. Each tattoo will feel like a pinprick. The tattoos will not be bigger than the head of a pin.
After they make the tattoos, your radiation therapists will take several photos of you in your simulation position. Your care team will use the photos and tattoos to position you correctly on the table each day of your treatment.
You can wash off the felt markings after your simulation. The tattoos are permanent and will not wash off. If you are concerned about having tattoos as part of your radiation treatment, talk with your radiation oncologist.
What to expect after your simulation
If you drank liquid contrast during your simulation, be sure to drink plenty of water for 24 hours after your simulation. Drinking water will help flush your kidneys.
Scheduling your radiation treatments
We will schedule your set-up procedure and first treatment at the end of your simulation appointment.
If you can’t come in for treatment for any reason, call your radiation oncologist’s office to tell your care team. If you need to change your schedule for any reason, speak with your radiation therapist or scheduler.
If you’re starting chemotherapy at the same time as radiation therapy, talk with the person scheduling your appointments when you’re starting your radiation therapy.
Treatment planning
Between your simulation and first treatment, your radiation oncologist will work with a team to plan your treatments. They will use your simulation scans to plan the angles and shapes of your radiation beams. They will also determine the dose of radiation that you will receive. These details are carefully planned and checked. This takes 7 to 10 business days.
What happens during radiation therapy to your pelvis
You’ll be in the same position for your radiation treatments as you were for your simulation. If pain or anxiety medicine was helpful for your simulation, you may want to take it before your radiation treatments. Take it about 1 hour before your appointment.
Wear comfortable clothes that are easy to take off. You will need to change into a hospital gown.
Your treatment appointments
Each day you have treatment, check in at the reception desk and have a seat in the waiting room. When your radiation therapists are ready for you, they will tell you to change into a hospital gown. Keep your shoes on.
Your radiation therapists will bring you into the treatment room and help you lie on the table. You will be positioned exactly how you were lying during your simulation.
Set-up procedure and first treatment
When you come in for your first treatment appointment, you’ll have imaging scans before your treatment starts. This is called a set-up procedure. It usually takes about 30 to 60 minutes.
Radiation treatments
You will have special images (x-rays or CT scans) taken during each of your treatment appointments. These are done to make sure your position and the area being treated is correct. They are not used to check how your tumor is responding to the radiation therapy.
Your radiation therapists will do their best to make sure you’re comfortable in your treatment position. Once everything is ready, they will leave the room and start your treatment.
Breathe normally during your treatment, but don’t move. You will not see or feel the radiation, but you may hear the machine as it moves around you and is turned on and off. You will be alone in the room during your treatment, but your radiation therapists will see you on a monitor and hear you through an intercom the whole time. Tell them if you’re uncomfortable or need help.
You will be in the treatment room for 10 to 30 minutes, depending on your treatment plan. Most of this time will be spent putting you in the correct position. The actual treatment only takes a few minutes.
Neither you nor your clothes will become radioactive during or after treatment. It is safe for you to be around other people and pets.
Status check visits
Your radiation oncologist or a radiation nurse will check in with you at least once during your radiation therapy. They’ll talk with you about any concerns, ask about any side effects you may be having, and answer your questions. This status check visit may be a telemedicine visit or a visit before or after your treatment.
If you need to speak with your radiation oncologist or radiation nurse outside your status check visit, call your radiation oncologist’s office. You can also ask the support staff or your radiation therapists to contact them when you come in for treatment.
Vitamins and dietary supplements during radiation therapy
It’s OK to take a multivitamin during your radiation therapy. Do not take more than the recommended daily allowance (RDA) of any vitamin or mineral.
Do not take any other dietary supplements without talking with a member of your care team. Vitamins, minerals, and herbal or botanical (plant-based) supplements are examples of dietary supplements.
Side effects of radiation therapy to your pelvis
Some people develop side effects from radiation therapy. The type and how severe they are depend on many factors. These include the dose of radiation, the number of treatments, and your overall health. Side effects may be worse if you’re also getting chemotherapy.
Below are the most common side effects of radiation therapy to the pelvis. You may have all, some, or none of these.
Diarrhea and rectal discomfort
Many people develop diarrhea (loose, watery bowel poop) within the first few weeks after starting radiation therapy. It’s also common to have cramping, pressure, and discomfort in your rectal area. You may also strain to have a bowel movement with no results.
There are some ways to help you manage these issues. Start following these guidelines if you start to have symptoms. Keep following them until your bowel movements go back to your usual pattern. This may take 2 to 4 weeks after your last treatment.
- Follow a diet that’s low in fiber, fat, and lactose (a sugar found in milk). Keep following this diet until your bowel movements go back to your usual pattern. You can then slowly go back to your usual diet.
- Drink more liquids to replace some of the water and salt you lose from having diarrhea. Try to drink 2 to 3 quarts (8 to 12 cups) of liquids throughout the day. Choose liquids such as Gatorade®, juices and nectars, non-fat soup broth, and Pedialyte®.
- Eat bananas and potatoes without the skin. They can help replace important nutrients you may lose from having diarrhea.
- Avoid any foods or drinks that makes your symptoms worse.
- Your radiation oncologist or nurse may tell you how to take medication for diarrhea. These instructions may be different from the instructions on the package.
- Take a sitz bath or tub bath to help relieve discomfort in your rectum. Use warm water and stay in the water no longer than 15 minutes at a time. You can take baths as often as you like for comfort.
- Take pain medicine if you have cramping or discomfort in your rectum. Your doctor will tell you what to take and how to take it.
Urinary changes
The lining of your bladder may become irritated during your radiation therapy. About 2 weeks after you start radiation therapy, you may need to urinate (pee) often and feel a burning sensation when you urinate. You may also feel an urgent need to urinate.
Here are some guidelines to help you manage these problems.
- Drink 2 to 3 quarts (8 to 12 cups) of liquids throughout the day.
- Avoid caffeine, alcohol, pepper, and spicy foods. These may irritate your bladder.
- Tell your radiation oncologist or nurse if you have any urinary changes. They can prescribe medication to help.
Skin and hair reactions
Your skin and hair in the treatment area may change during your radiation therapy. This is normal.
- After 2 to 3 weeks, your skin may become pink or tanned. Later on, it may become bright red or very dark, based on your skin tone.
- Your skin may feel dry and itchy and look flaky. The skin in sensitive areas (such as your groin, vaginal area, testicles, penis, or scrotum) may blister, open, and peel. If this happens, tell a member of your care team.
- You may lose some or all of your hair in the treatment area. Hair most often grows back 2 to 4 months after you finish radiation therapy.
If you develop a severe (very bad) reaction, your nurse will apply special dressings or creams and teach you how to care for your skin. Your skin will gradually heal, but it may take 3 or 4 weeks after you finish radiation therapy.
Your radiation oncologist may prescribe a medicine to treat itchy skin. They may prescribe it when you start radiation therapy or after a few treatments.
The guidelines below can help you care for your skin during your radiation therapy. Follow them until your skin gets better. These guidelines are only for your skin in the radiation treatment area. You can care for the rest of your skin as usual.
Keep your skin clean
-
Bathe or shower every day.
- Use warm water and a mild unscented soap, such as Neutrogena®, Dove®, baby soap, Basis®, or Cetaphil®.
- Be gentle with your skin when you wash it. Do not use a washcloth, loofah, or brush.
- Rinse your skin well.
- Pat your skin dry with a soft, clean towel.
- Your radiation therapists may outline your treatment area with a purple felt-tipped marker. You can remove these markings with mineral oil when your radiation therapists say it’s OK.
- Do not use alcohol or alcohol pads on your skin.
Moisturize your skin often
- If you’re likely to get a skin reaction, your nurse will recommend that you start using a moisturizer. Start using it the first day of your radiation therapy to minimize the reaction.
- If you’re not likely to develop a skin reaction, you will not need a moisturizer unless your skin becomes dry or itchy. Your nurse will give you instructions.
- If you aren’t sure if you should use a moisturizer, ask your nurse.
If your nurse tells you to use a moisturizer:
- Moisturize your skin 2 times every day.
- Use a moisturizer without fragrances or lanolin. Lanolin is an oil made by animals that have wool, such as sheep. It can make your skin more sensitive. There are many over-the-counter (not prescription) moisturizers that are good to use. Your nurse may suggest one. If you’re not sure which one to use, ask your radiation nurse.
- Only use 1 moisturizer at a time unless your radiation nurse tells you to use more.
Avoid irritating your skin
- Wear loose-fitting cotton clothing. Do not wear tight clothing that will rub against your skin.
- Use only the moisturizers, creams, or lotions your radiation oncologist or nurse suggests.
- Do not put anything sticky (such as Band-Aids® or medical tape) on your skin.
- Do put any patches on your skin, including pain patches.
- If your skin is itchy, do not scratch it. Ask your nurse for recommendations on how to ease the itching.
- Avoid shaving your skin. If you must shave, use an electric razor. Stop if your skin becomes irritated
- Do not expose your skin to very hot or cold temperatures. For example, do not use hot tubs, hot or cold water bottles, heating pads, or ice packs.
- Only swim in a pool if you do not have any skin reactions. Rinse off right after you get out.
- Avoid tanning or burning your skin. If you’re going to be in the sun, use a sunblock with an SPF of 30 or higher. Wear loose-fitting clothing over as much of your skin as you can.
Fatigue
Fatigue is feeling very tired or weak. When you feel fatigued, you may not want to do things. You may have trouble focusing, feel slowed down, or have less energy than usual. Fatigue can range from mild (not bad) to severe (very bad). It may be worse at certain times of day.
You may start to feel fatigued after 2 to 3 weeks of treatments. You may still feel fatigued for a few weeks to several months after finishing radiation therapy. Fatigue usually gets better over time.
There are lots of reasons you may feel fatigued during your radiation therapy. They include:
- The radiation’s effects on your body.
- Traveling to and from your treatment appointments.
- Not getting enough restful sleep at night.
- Not getting enough protein and calories.
- Having pain or other symptoms.
- Feeling anxious (nervous) or depressed (unhappy).
- Side effects of some medicines.
Ways to manage fatigue
- If you’re working and are feeling well, it’s OK to keep working. But working less may help you have more energy.
- Plan your daily activities. Pick the things you need or really want to do. Do them when you have the most energy. For example, you may choose to go to work but not do housework. You may choose to watch your child’s after-school event but not go out to dinner.
- Plan time to rest or take short (10- to 15-minute) naps during the day, especially when you feel more tired.
-
Try to sleep at least 8 hours every night. This may be more sleep than you needed before you started radiation therapy. You may find it helpful to:
- Go to sleep earlier and get up later.
- Be active during the day. For example, if you’re able to exercise, you could go for a walk or do yoga.
- Relax before going to bed. For example, read a book, work on a puzzle, listen to music, or do another calming hobby.
- Ask family and friends to help with chores and errands. Check with your health insurance company to see if they cover home care services.
- You might have more energy when you exercise. Ask your radiation oncologist if you can do light exercise, such as walking, biking, stretching, or yoga. Read Managing Cancer-Related Fatigue with Exercise to learn more.
- Eat foods that are high in protein and calories. Read Eating Well During Your Cancer Treatment to learn more.
Some things can make your fatigue worse. Examples are:
- Pain
- Nausea (feeling like you’re going to throw up)
- Diarrhea (loose or watery poop)
- Trouble sleeping
- Feeling depressed or anxious
Ask your radiation oncologist or nurse for help if you have these or any other symptoms or side effects.
Changes to your blood cell counts
Bone marrow is the substance inside your bones that makes blood cells. You have 3 kinds of blood cells. White blood cells fight off infection. Platelets help your blood to clot when you injure yourself. Red blood cells carry the oxygen you need for energy.
You may have lowered blood cell counts (lower levels of blood cells) when large areas of bone marrow are in the area being treated. If you’re also getting chemotherapy, it can also affect your blood cell count.
We may monitor you throughout your radiation therapy with a blood test called a complete blood count (CBC). If your counts drop, we may stop your radiation therapy until the level increases. Your care team will talk with you about what to expect.
Appetite loss
Some people find that their appetite decreases during radiation therapy. Your body needs protein and calories to repair the normal cells injured from radiation therapy. Try not to lose weight during your radiation therapy. Below are suggestions to help you maintain your weight.
- Eat foods and drink liquids that are high in protein and calories. Your nurse will give you Eating Well During Your Cancer Treatment, or you find it online.
- Try to eat small meals often throughout the day. If you never seem to feel hungry, make a schedule to make sure you eat regularly, for example every 2 hours.
- Eat your meals in a calm place and take your time. Eat with family or friends whenever possible.
- Vary the color and texture of your foods to make them more appealing.
- Bring snacks and drinks with you when you come for treatment. You can have these while you’re waiting or while you’re coming to and from your treatments.
- You can drink liquid nutritional supplements if you’re not eating enough food. There are many products available and they come in many flavors. Ask your doctor or nurse which product is best for you.
Sexual and reproductive health
You are not radioactive. You can’t pass radiation to anyone else. It’s safe to be in close contact with other people.
You can be sexually active during your radiation therapy, unless your radiation oncologist gives you other instructions. If if you or your partner are able to have children, you must use contraception (birth control) to prevent pregnancy during your radiation therapy.
Information for people born with testicles
If you get someone pregnant with sperm damaged by exposure to radiation, there is a risk of miscarriage or birth defects. If your partner could become pregnant, use contraception (birth control) during your radiation therapy.
Sexual changes
During radiation therapy, some people have a burning sensation when they ejaculate. For most people, it goes away 1 or 2 months after finishing radiation therapy.
Some people develop sexual changes after finishing radiation therapy, including:
- Less firm (hard) erections.
- An inability to get an erection.
- A change in how orgasms feel.
- A change in the amount or texture of semen when you ejaculate.
These changes may happen many months or even years after radiation therapy. They may be permanent, but you will have options to treat them. Your doctor or nurse can give you a referral to a doctor who treats these issues.
If you need more help or support, contact the Male Sexual & Reproductive Medicine Program at 646-888-6024.
Information for people born with ovaries and a uterus
Vaginal changes
Your vagina may become irritated during your radiation therapy. About 2 weeks after starting radiation therapy, you may notice a vaginal discharge (fluid that comes out of your vagina). This may last for 2 to 4 weeks after you finish radiation therapy.
Follow these suggestions to manage any discomfort.
- Take sitz baths or tub baths in warm water. Don’t stay in the water longer than 15 minutes at a time. You can take these baths as often as you like for comfort.
- Use panty liners to manage vaginal discharge. Do not use tampons.
- If your labia are itchy or irritated, apply the moisturizer your nurse gave you.
- Talk with your doctor or nurse before douching. Douching may make the irritation worse.
- Talk with your doctor or nurse about having vaginal intercourse (sex that involves putting something in your vagina). You may need to wait for your vaginal tissues to heal. If you are having vaginal intercourse, use a vaginal lubricant (such as Astroglide® or K-Y® Jelly) to increase your comfort. Use a condom to help prevent a vaginal infection.
- If you need to use a vaginal dilator, your radiation therapy team will discuss this with you and give you more information.
If you need more help or support, contact the Female Sexual Medicine & Women’s Health Program at 646-888-5076.
Hormonal changes
If your ovaries are in the area being treated, your ovarian function may be affected. If you have not yet started menopause, your periods may stop and you may start menopause. You may develop symptoms such as hot flashes, insomnia, and mood swings.
Tell your doctor or nurse if these symptoms bother you. They can refer you to a gynecologist to discuss options to decrease these symptoms.
Fertility
If you can get pregnant, you must use contraception (birth control) to prevent pregnancy during your radiation therapy.
Sexual health programs
MSK offers sexual health programs. These programs can help you manage the ways your cancer or cancer treatment affect your sexual health or fertility. Our specialists can help you address sexual health or fertility issues before, during, or after your radiation therapy.
- For information about our Female Sexual Medicine & Women’s Health Program or to make an appointment, call 646-888-5076.
- For information about our Male Sexual & Reproductive Medicine Program or to make an appointment, call 646-888-6024.
- For information about our Cancer and Fertility Program, talk with your healthcare provider.
Other resources
For more information about your sexual health during cancer treatment, read Sex and Your Cancer Treatment.
The American Cancer Society also has resources about sexual health issues during cancer treatment. They’re called Sex and the Adult Male with Cancer and Sex and the Adult Female with Cancer. You can search for them at www.cancer.org or call 800-227-2345 for a copy.
Emotional health
|
|
|
You might also worry about telling your employer you have cancer or about paying your medical bills. You may worry about how your family relationships may change, or that the cancer will come back. You may worry about how cancer treatment will affect your body, or if you will still be sexually attractive.
It’s normal and OK to worry about all these things. All these kinds of feelings are normal when you or someone you love has a serious illness. We’re here to support you.
Ways to cope with your feelings
Talk with others. When people try to protect each other by hiding their feelings, they can feel very alone. Talking can help the people around you know what you’re thinking. It might help to talk about your feelings with someone you trust. For example, you can talk with your spouse or partner, close friend, or family member. You can also talk with a chaplain (spiritual advisor), nurse, social worker, or psychologist.
Join a support group. Meeting other people with cancer will give you a chance to talk about your feelings and learn from others. You can learn how other people cope with their cancer and treatment and be reminded you’re not alone.
We know that all cancer diagnoses and people with cancer are not the same. We offer support groups for people who share similar diagnoses or identities. For example, you can join a support group for people with breast cancer or for LGBTQ+ people with cancer. Visit www.msk.org/vp to learn about MSK’s support groups. You can also talk with your radiation oncologist, nurse, or social worker.
Try relaxation and meditation. These kinds of activities can help you feel relaxed and calm. You might try thinking of yourself in a favorite place. While you do, breathe slowly. Pay attention to each breath or listen to soothing music or sounds. For some people, praying is another way of meditation. Visit www.msk.org/meditations to find guided meditations lead by our Integrative Medicine and Wellness providers.
Exercise. Many people find that light movement, such as walking, biking, yoga, or water aerobics, helps them feel better. Talk with your healthcare provider about types of exercise you can do.
We all have our own way of dealing with tough situations. Often, we do what worked for us in the past. But sometimes that’s not enough. We encourage you to talk with your doctor, nurse, or social worker about your concerns.
What happens after radiation therapy to your pelvis
Follow-up appointments
It’s important to come to all your follow-up appointments with your radiation oncologist. During these appointments, they will check how you’re recovering after your radiation therapy.
Write down your questions and concerns before your follow-up appointments. Bring this and a list of all your medicines with you. You can also call your radiation oncologist or nurse any time after you finish radiation therapy or between follow-up appointments.
Vitamins and dietary supplements after radiation therapy
- You might be getting other cancer treatments along with your radiation therapy. If you are, ask the doctor managing that treatment when it’s safe to start taking dietary supplements again. Some dietary supplements are not safe to take before surgery or during chemotherapy.
- If you are not getting other cancer treatments, you can start taking dietary supplements again 1 month after your last radiation treatment.
Tell your radiation nurse if you want to talk with a clinical dietitian nutritionist about your diet or supplements.
When to call your healthcare provider
Call your radiation oncologist or nurse if you have:
- A fever of 100.4 °F (38 °C) or higher.
- Chills.
- Black or bloody bowel movements.
- Dizziness.
- Flu-like symptoms, such as a headache, cough, sore throat, body aches, or a fever.
- Vaginal bleeding.
- Blood in your urine.
- Any new or unusual symptoms.
Support services
MSK support services
Counseling Center
www.msk.org/counseling
646-888-0200
Many people find that counseling helps them. Our counseling center offers counseling for individuals, couples, families, and groups. We can also prescribe medicines to help if you feel anxious or depressed. Ask your healthcare provider for a referral or call the number above to make an appointment.
Integrative Medicine and Wellness Service
www.msk.org/integrativemedicine
Our Integrative Medicine and Wellness Service offers many services to complement (go along with) traditional medical care, including music therapy, mind/body therapies, dance and movement therapy, yoga, and touch therapy. Call 646-449-1010 to schedule an appointment for these services.
You can also schedule a consultation with a healthcare provider in the Integrative Medicine and Wellness Service. They will work with you to come up with a plan for creating a healthy lifestyle and managing side effects. Call 646-608-8550 to make an appointment.
Nutrition Services
www.msk.org/nutrition
212-639-7312
Our Nutrition Service offers nutritional counseling with one of our clinical dietitian nutritionists. Your clinical dietitian nutritionist will talk with you about your eating habits. They can also give advice on what to eat during and after treatment. Ask a member of your care team for a referral or call the number above to make an appointment.
Rehabilitation Services
www.msk.org/rehabilitation
Cancers and cancer treatments can make your body feel weak, stiff, or tight. Some can cause lymphedema (swelling). Our physiatrists (rehabilitation medicine doctors), occupational therapists (OTs), and physical therapists (PTs) can help you get back to your usual activities.
- Rehabilitation medicine doctors diagnose and treat problems that affect how you move and do activities. They can design and help coordinate your rehabilitation therapy program, either at MSK or somewhere closer to home. call Rehabilitation Medicine (Physiatry) at 646-888-1929 to learn more.
- An OT can help if you’re having trouble doing usual daily activities. For example, they can recommend tools to help make daily tasks easier. A PT can teach you exercises to help build strength and flexibility. Call Rehabilitation Therapy at 646-888-1900 to learn more.
Resources for Life After Cancer (RLAC) Program
646-888-8106
At MSK, care does not end after your treatment. The RLAC Program is for patients and their families who have finished treatment.
This program has many services. We offer seminars, workshops, support groups, and counseling on life after treatment. We can also help with insurance and employment issues.
Sexual Health Programs
Cancer and cancer treatments can affect your sexual health, fertility, or both. MSK’s sexual health programs can help you before, during, or after your treatment.
- Our Female Sexual Medicine & Women’s Health Program can help with sexual health problems such as premature menopause or fertility issues. Ask a member of your MSK care team for a referral or call 646-888-5076 to learn more.
- Our Male Sexual & Reproductive Medicine Program can help with sexual health problems such as erectile dysfunction (ED). Ask a member of your care team for a referral or call 646-888-6024 to learn more.
Tobacco Treatment Program
www.msk.org/tobacco
212-610-0507
MSK has specialists who can help you quit smoking. Visit our website or call the number above to learn more. You can also ask your nurse about the program.
Virtual Programs
www.msk.org/vp
Our Virtual Programs offer online education and support for patients and caregivers. These are live sessions where you can talk or just listen. You can learn about your diagnosis, what to expect during treatment, and how to prepare for your cancer care.
Sessions are private, free, and led by experts. Visit our website for more information about Virtual Programs or to register.
Radiation therapy support services
American Society for Therapeutic Radiology and Oncology
www.rtanswers.org
800-962-7876
This website has detailed information about treating cancer with radiation. It also has contact information for radiation oncologists in your area.
External support services
There are many other support services to help you before, during, and after your cancer treatment. Some offer support groups and information, while others can help with transportation, lodging (a place to stay), and treatment costs.
For a list of these support services, read External Support Services. You can also talk with an MSK social worker by calling 212-639-7020.
Questions to ask your radiation oncologist
Before your appointment, it’s helpful to write down questions you want to ask. Examples are listed below. Write down the answers during your appointment so you can review them later.
What kind of radiation therapy will I get?
How many radiation treatments will I get?
What side effects should I expect during my radiation therapy?
Will these side effects go away after I finish my radiation therapy?
What kind of late side effects should I expect after my radiation therapy?