Bottom Line:
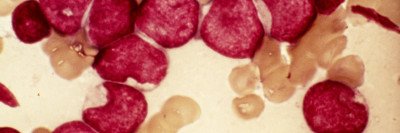
Drug resistance is a formidable challenge in cancer treatment. A drug called enasidenib (Idhifa®) was approved by the US Food and Drug Administration last year for the treatment of people with a form of acute myeloid leukemia (AML) that’s driven by a mutation in the gene IDH2. About 15 percent of people with AML have this mutation. Research led by Memorial Sloan Kettering Cancer Center (MSK) reports that people who take enasidenib can develop resistance to it — in a way never seen before. Enasidenib works differently than most cancer drugs. Rather than killing leukemia cells, it turns them into normal blood cells. The discovery of this unique resistence may lead to more-precise treatments for people with AML in the future.
Findings:
This important discovery was made by a team of doctors, laboratory researchers, and pharmaceutical company scientists. They used cells from people who were being treated with enasidenib to uncover why the drug sometimes stops working. The findings suggest that some people may develop resistance to IDH inhibitors due to a mutation on the same copy of the gene that carries the cancer-causing mutation.
Journal:
The paper, “Acquired resistance to IDH inhibition through trans or cis dimer-interface mutations,” appears in the July 5, 2018, issue of Nature.
Authors:
Memorial Sloan Kettering’s Eytan Stein, MD, led the pivotal clinical trial that resulted in the drug’s approval, and he and MSK’s Ross Levine, MD, were the paper’s co-senior authors; MSK’s first author was Andrew Intlekofer, MD, PhD.
Background:
IDH2 mutations and mutations in the related gene IDH1 are found in other types of leukemia as well as myelodysplastic syndrome, glioblastoma, and bile duct cancer.
Researchers had previously shown that only one of the two copies of the IDH2 gene needs to be mutated to drive cancer. The other one is usually normal. In the new paper, the investigators report that when cells developed resistance to enasidenib, the additional mutations that allowed the cells to resist the drug occurred on the normal copy of IDH2.
Two patients were in the study, but the investigators learned a great deal. Experiments with laboratory models allowed them to study how the mutations work. After the people in the study developed resistance, their tumors started growing again. Doctors were able to switch them to other drugs that worked in a different way, however, so they were not affected by the additional mutation. There are a number of other treatment options for people with AML. These include both FDA-approved therapies and experimental drugs being tested in clinical trials. Many people with AML ultimately receive stem cell or bone marrow transplants, which offer the opportunity for a cure. However, some people are not able to undergo transplants, which makes developing new drugs an important focus.
Author Comments:
“Everyone who studies precision medicine spends a lot of time thinking about why some people respond to certain drugs and why some stop responding or never respond at all,” said physician-scientist Dr. Levine, who was one of the paper’s senior authors, along with Dr. Stein. “MSK has been one of the leaders in figuring this out.”
“Now that we know resistance to enasidenib can develop, we can start to monitor people for it by conducting blood tests,” said first author Dr. Intlekofer, who is also a physician-scientist in MSK’s Human Oncology and Pathogenesis Program. “Over the course of therapy, we can use the protein as a biomarker for the formation of resistance. Then we’ll know we need to offer a different treatment.”
“It’s really a transformation. Patients will go from being riddled with infections to having a normally functioning body,” said senior corresponding author and MSK medical oncologist Dr. Stein. “We’ve been driving a lot of the clinical development and also the correlative science to understand what’s happening in patients.”
Funding:
The study was funded by the National Cancer Institute grants K08 CA201483, K08 CA181507, R01 CA168802-02, R35 CA197594-01A1, U54 OD020355, and P30 CA008748; the Leukemia and Lymphoma Society; the Burroughs Wellcome Fund; the Susan and Peter Solomon Divisional Genomics Program; the Steven A. Greenberg Fund; the Translational and Integrative Medicine Research Fund; the American Association for Cancer Research; the American Society of Hematology/Robert Wood Johnson Foundation; Cycle for Survival; and the Marie-Josée and Henry R. Kravis Center for Molecular Oncology.