
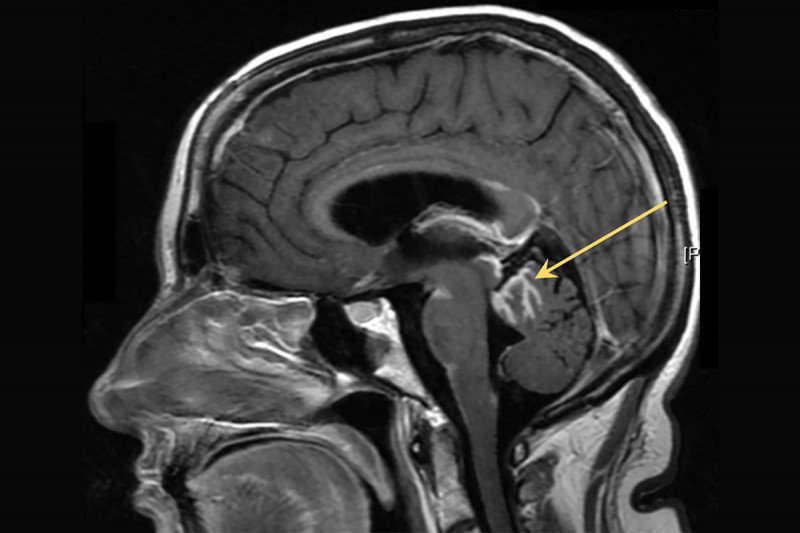
Cancer that spreads to the fluid and tissues surrounding the brain and spinal cord can have devastating effects. The condition, called leptomeningeal metastasis, may cause pain, seizures, difficulty thinking, and a loss of muscle, bowel, and bladder control. In the past 20 years, it’s become more common because people are living longer after treatment of their primary tumors.
Current treatments for leptomeningeal metastasis are chemotherapy and radiation therapy, but neither is very effective at destroying the cancer cells. One reason is that this fluid, called cerebrospinal fluid (CSF), is largely sealed off from the rest of the body by a tight barrier. Normally this barrier protects the brain and spinal cord, but when cancer cells manage to invade the space, it’s hard for treatments like chemotherapy to penetrate. Radiation therapy is difficult to give without damaging the spinal cord or brain function.
In addition, doctors have been puzzled by how the cancer cells grow in CSF. There is a dearth of iron in the area that cancer cells rely on to support their growth. It has been a bit of a mystery how the cells survive in this barren environment — they seem to defy the odds and have no obvious weak spot to target.
Now a team of Memorial Sloan Kettering researchers led by neuro-oncologist Adrienne Boire may have found the cancer cells’ secret power: They reprogram themselves to gobble up all the nearby iron. By hogging this nutrient, the cancer cells ensure they stay alive and grow while other cells — notably immune cells that have entered the same space — are left short.
“It’s an elegant solution on the part of the cancer cell,” Dr. Boire says. “It’s really unique biology that allows them to win the competition.” The researchers published their discovery on July 16 in Science. They say the finding also points to a possible strategy for treatment.
Genomic Toolbox
To investigate how cancer cells survive in CSF, the researchers analyzed fluid samples taken from five patients with leptomeningeal metastasis. They collaborated with the laboratory of Dana Pe’er to conduct a test called single cell RNA sequencing of the cancer cells in the fluid.
The analysis revealed that the cancer cells increase their activity of a gene called Lipocalin-2. The protein made by this gene binds iron. Immune cells use this protein too, when they are fighting bacteria. But in the CSF, the cancer cells boost their Lipocalin-2 protein levels to outcompete the immune cells for iron in the surroundings. It’s like creating a stronger magnet than the immune cells to pick up more paper clips.
“It’s nefarious, the way the cancer cells exploit Lipocalin-2 to gain an advantage over the immune cells,” Dr. Boire explains. The cancer cell can look through its genome — the entire set of DNA — and deploy the genes that give it a critical survival advantage. The immune cells in the CSF, by contrast, are hamstrung. They lack the ability of the cancer cells to access different parts of the genomic toolbox.
Knowing that iron plays such a key role in leptomeningeal metastasis led the researchers to their next question: What if you could cut off access to iron and starve the cancer cells? In mouse models for the disease, they tested whether the iron could be bound with chemical compounds called iron chelators. They delivered the chelators directly into the spinal fluid. As hoped, this slowed the growth of the cancer cells.
“It reminds me of when two kids are fighting over a toy, and the parent says, ‘That’s it — I’m taking it away. Nobody gets it,’” Dr. Boire says.
Broader Questions
The researchers are working to bring this therapy to a clinical trial. They think the treatment will be safe if the chelators don’t escape the CSF. “When cancer gets in the CSF, it is sealed away in its own ecosystem, which is why it’s hard to treat. But if you can deliver drugs into that space, the treatments don’t go anywhere else, so side effects are limited.”
Dr. Boire says the discovery also raises intriguing questions about why immune cells may behave differently around the brain and spinal cord. Normally, immune cells can produce Lipocalin-2 and compete for iron, so something is disabling them.
“If we find out, we could possibly help patients with central nervous system cancers benefit from immune therapies, which often don’t work in the nervous system for reasons we don’t understand,” Dr. Boire says. “This is potentially important for cancer research and cancer biology. That’s how science goes — you’re looking in one direction and then you uncover a corner of something that’s really interesting.”





