As leaders in immunotherapy, Memorial Sloan Kettering researchers have spent decades studying how the immune system responds to cancer. During the COVID-19 pandemic, many of them are applying their insights toward gaining a deeper understanding of how the immune system reacts to the coronavirus that causes COVID-19.

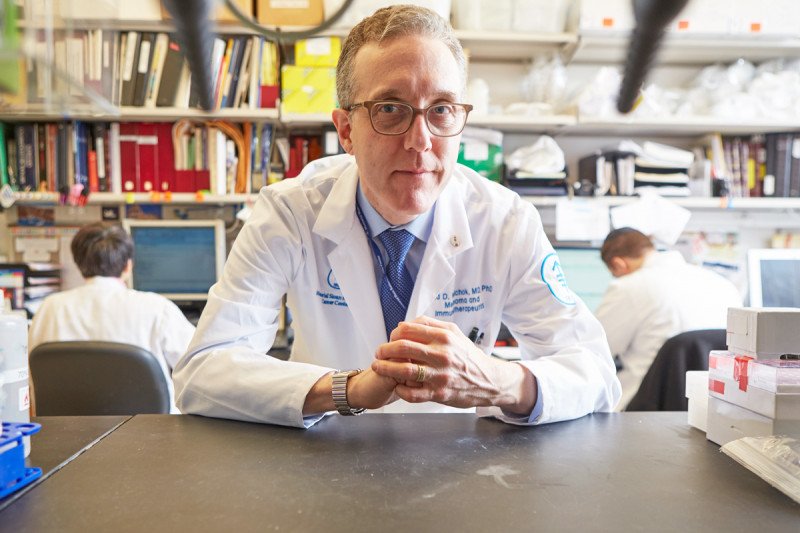
In an article published April 30 in the Journal of Experimental Medicine, MSK physician-scientists Jedd Wolchok and Santosha Vardhana share what they’ve learned on the front lines of caring for people with both cancer and COVID-19. They explain how the immune system’s response leads to the symptoms of COVID-19. They also outline how that response has pointed to potential therapies for COVID-19. Some of these treatments are already being tested in clinical trials at MSK and other hospitals.
“We are still in the early stages of understanding COVID-19, both clinically and on a more basic science level,” Dr. Wolchok says. “We wrote this paper to describe what we’ve learned about the very complicated relationship that this virus has with the immune system.”
He adds, “In the longer term, vaccines are going to be extremely important for durable control of the pandemic. But since we don’t know how long it will take to develop a vaccine, we need to find the best way to treat individuals who are already infected.”
A Two-Part Process for Attacking COVID-19
An immune response has two stages. The first, called innate immunity, begins the instant the body senses any kind of infection. During the innate immune response, several types of immune cells rush to the sight of infection and attempt to tamp down the invader. In COVID-19, the innate immune response is responsible for some symptoms, including fever, headache, and cough.
The second part of the immune response is acquired immunity. This happens when the body begins to make antibodies against a specific invader. “Antibodies help your immune system remember the virus if it ever comes back,” Dr. Vardhana explains. “But the other part of acquired immunity is how your immune cells coordinate the repair of tissues that have been damaged by the infection. This has not been well studied in COVID-19.
“While caring for people with COVID-19, I saw that many of them were having problems with the tissue repair part of the immune response,” Dr. Vardhana continues. “They just weren’t getting better, and the longer they were sick, the harder it was for their immune systems to fight back.” He realized these patients were lacking alveolar macrophages, a type of immune cell that’s important for repairing the kind of lung damage that often results from COVID-19.
Rapidly Moving Discoveries to the Clinic
Based on ongoing research that Dr. Vardhana has been conducting as a member of MSK President and CEO Craig Thompson’s lab, he was able to identify a drug that might help replenish alveolar macrophages, called N-acetylcysteine. This drug is currently approved for repairing the liver after acetaminophen (Tylenol®) overdose. It’s also used to treat lung damage seen in people with cystic fibrosis.
A trial looking at whether N-acetylcysteine can repair lung tissue in people recovering from COVID-19 is already underway at MSK. “We know this drug can be administered safely in people with lung damage, and it’s likely to provide benefit,” says Dr. Vardhana, who is leading the study together with Dr. Wolchok. “The fact that we were able to get this trial approved so quickly is a testament to efforts across the whole institution.”
MSK investigators have launched another clinical trial for treating COVID-19 in people with cancer. This study, led by bone marrow transplant (BMT) specialists Boglarka Gyurkocza and Ann Jakubowski, targets the immune response. Based on early reports, doctors suspect that some of the lung damage in COVID-19 is caused by an exaggerated inflammation reaction from the immune system. The trial is looking at tocilizumab (Actemra®), a drug that’s already approved to treat cytokine release syndrome, the extreme immune reaction seen in some people getting chimeric antigen receptor T cell therapy.
“We are hoping to minimize damage to the lung and other organs associated with COVID-19. This drug targets one of the inflammatory molecules that can be substantially elevated in people with COVID-19 infections,” Dr. Gyurkocza says. “I believe a combination of different approaches, such as targeting the virus directly, modulating the immune response, and enhancing tissue repair, will result in substantial improvements for patients. I’m impressed by the plethora of ideas my colleagues at MSK are coming up with.”
A third trial is currently under review and expected to launch soon. It aims at increasing the number of immune cells called T cells, part of the acquired immune response. The trial will focus on an experimental drug called interleukin-7 (IL-7), which has been studied at MSK as a way to boost T cell production after a BMT and in people with severe sepsis. T cell function becomes depressed in people with COVID-19 and is associated with high mortality. By increasing the number of viral-specific T cells, IL-7 may be effective in improving a patient’s ability to eradicate the virus.
That trial will be led by Stephen Pastores, Director of the Critical Care Medicine Fellowship Training and Research Programs, in collaboration with physician-scientist Marcel van den Brink and Miguel-Angel Perales, Chief of the Adult Bone Marrow Transplant Service, who both have studied IL-7 in people recovering from BMTs.
“Caring for people with COVID-19 gave me a real sense of all the barriers these patients are facing,” Dr. Vardhana says. “We’ll now be able to offer people different trials, depending on their individual situations.”
Drs. Wolchok and Vardhana credit the Parker Institute for Cancer Immunotherapy (PICI) for enabling and supporting much of the fundamental research that’s being done on COVID-19, not only at MSK but at other cancer centers across the country. “PICI has really jumped in to bring together expertise to better understand the many faces of the immune response to COVID-19,” Dr. Wolchok concludes.






