When it comes to giving immunotherapy to people with the most common form of lymphoma, the time of day may make a difference, according to new research from Memorial Sloan Kettering Cancer Center (MSK).
People who receive chimeric antigen receptor (CAR) T cell therapy in the morning may be more likely to have a good response than those who receive it later in the day, the international study finds. Although the research is preliminary, it suggests giving CAR T cell therapy based on the body’s circadian rhythms may be a way to further improve outcomes for some patients.
The study focused on patients who had received CAR T therapy for large B cell lymphoma, which makes up about one-third of non-Hodgkin lymphoma cases. The paper was published January 5, 2026, in the journal Blood.
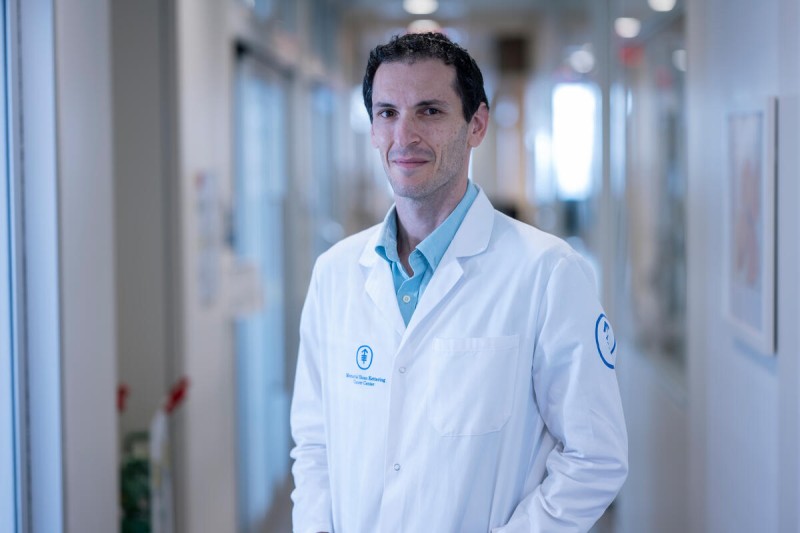
“The link between circadian rhythms and treatment effectiveness is a relatively new area of research,” says MSK bone marrow transplant specialist and cellular therapist Roni Shouval, MD, PhD, co-corresponding author of the paper. “By studying this connection, we hope to improve the way CAR T therapy is administered, so that more people can benefit from this potentially lifesaving therapy.”
What Is CAR T Therapy and How Does It Work?
CAR T therapy is a type of immunotherapy pioneered by MSK in the early 2000s, when researchers engineered the first cells that were able to survive, proliferate, and kill cancer cells in the lab. Since then, several CAR T therapies have been approved to treat patients with lymphoma and other blood cancers. They are also being studied for treating solid tumors.
With CAR T therapy, a patient’s T cells (white blood cells that are crucial for fighting disease) are collected and sent to a lab, where they are engineered to more effectively recognize cancer cells. They are then infused back into the patient, so they can seek out and destroy the cancer.
Scientists have been searching for new ways to make CAR T more successful for more patients. The success rate of CAR T therapy varies. Between 50% and 90% of patients with lymphoma, leukemias, and other blood cancers who receive these treatments go into remission, but achieving a long-lasting response remains a challenge.
Why Did Researchers Study the Timing of CAR T Therapy?
Scientists have learned that circadian rhythms — the body’s natural 24-hour cycles — affect not only sleep patterns, but also hormone levels, metabolism, and the immune system.
“Previous studies revealed that other types of immunotherapy, like immune checkpoint inhibitors, may work better when they are given earlier in the day,” says Dr. Shouval, Director of MSK’s Precision Cellular Therapy Laboratory. “Although the timing of CAR T therapy has been studied in mouse models, to our knowledge, this is the first large analysis to look at connections between patient outcomes and the time of day that CAR T therapy is given.”
Dr. Shouval is an internationally recognized expert on what causes disease to become resistant to cellular therapies.
Study Results: Time-of-Day of CAR T Cell Infusion and Outcomes in Large B Cell Lymphoma
The team reviewed medical records from more than 1,000 patients who received a CAR T treatment between 2017 and 2025. The patients were treated at seven different hospitals in the United States, Europe, and Israel. Geographic diversity was important to ensure that the location of the hospital was not a factor in the patients’ outcomes, the researchers say.
The data analysis included the time of day the treatment was given, how patients responded immediately after the treatment, and how likely the cancer was to return over time.
Overall, the analysis revealed that:
- For patients who got their treatment before noon, 51% had progression-free survival at one year, meaning their cancer had not come back.
- For those who got their treatment after noon, only 35% had progression-free survival at one year.

“We found that patients who got their treatment later in the day had lower levels of CAR T expansion, which means that the engineered cells did not proliferate as effectively in their bodies,” says co-corresponding author Kai Rejeski, MD, MHBA, an affiliated member of Dr. Shouval’s lab who leads an independent research group at the Ludwig Maximilian University in Munich.
“Patients who got treated later in the day also had higher levels of pathologic inflammation following infusion,” Dr. Rejeski notes, “which may in part explain the inferior outcomes.”
What Determines the Timing of CAR T Therapy?
The first author of the Blood paper, Danny Luan, MD, a fellow in Dr. Shouval’s lab, noted that there may be several logistical reasons why CAR T recipients receive their infusions later. For example, they may be treated in the afternoon instead of the morning because they need to get scans or blood transfusions first. Also, the infusion may depend on what time the cells are delivered to the clinic from the lab where they are made.
If additional studies confirm the benefits of giving CAR T therapy early in the day, doctors could work to optimize the process according to patients’ circadian rhythms.
Dr. Shouval says it may eventually be possible to give patients drugs that affect the body’s circadian rhythms, to boost the effectiveness of CAR T and other immunotherapies.
What Are the Next Steps for Research on CAR T Therapy and Circadian Rhythms?
It is important to note that this study was retrospective and showed only a correlation, not direct causation. To confirm the findings, researchers need to conduct prospective studies specifically designed to determine the differences in outcomes based on treatment times.
Future studies will also include data on what time of day the patient’s T cells are collected before the engineering process. “It’s very likely this could affect the makeup and quality of the T cells,” Dr. Rejeski says.
Additional Authors, Funding, and Disclosures
In addition to MSK, the other hospitals that treated patients in the study were Chaim Sheba Medical Center in Tel HaShomer, Israel; Hackensack University Hospital in Hackensack, New Jersey; LMU University Hospital in Munich; Rambam Health Care Campus in Haifa, Israel; Soroka University Medical Center in Be’er Sheva, Israel; and Tel Aviv Sourasky Medical Center in Tel Aviv, Israel. A full list of authors and participating research institutions is available in the paper.
This research was supported in part by National Institutes of Health grant P01 CA23766 and National Institutes of Health/National Cancer Institute grant P30 CA008748. Dr. Shouval reports grant support from NIH-NCI K08-CA282987 and an award from the Long Island Sound Chapter, Swim Across America. Dr. Rejeski acknowledges support from a grant by the Bruno and Helene Jöster Foundation and the CAR T Control translational group within the Bavarian Center for Cancer Research (BZKF-#TLG-22).
Dr. Shouval’s disclosures are available on his webpage.
Key Takeaways
- New research from Memorial Sloan Kettering Cancer Center (MSK) finds that circadian rhythms — the body’s natural 24-hour cycles — may affect how patients respond to cancer treatment.
- The international study suggests that people who get CAR T therapy in the morning respond better than people who get their treatment in the afternoon.
- This finding is based on a retrospective analysis of medical records from patients who received CAR T between 2017 and 2025 at hospitals in the U.S., Europe, and Israel — more research is needed to confirm the results.
- If the findings are confirmed, it could lead to new ways to optimize CAR T treatments so that more people can benefit from them.