If you’re worried you have bladder cancer, you probably have many questions.
What causes bladder cancer? What are the symptoms and early signs of bladder cancer? How do we diagnose bladder cancer? How fast does bladder cancer spread?
MSK’s guide to bladder cancer is a good place to start finding answers. We explain what bladder cancer is, and describe common types, such as non-invasive bladder cancer. We also explain the latest treatments, such as antibody-drug conjugate therapy and immunotherapy, including bacillus Calmette-Guérin (BCG) treatment.
- What is bladder cancer?
- What are the types of bladder cancer?
- What are the symptoms of bladder cancer?
- What are the risk factors for bladder cancer?
- How is bladder cancer diagnosed?
- What are the treatments for bladder cancer?
- Why should I choose Memorial Sloan Kettering for bladder cancer treatment?
What is bladder cancer?
Bladder cancer often is thought of as a disease of older men. That’s because more men get bladder cancer, and they often get it after age 70. But younger people can get the disease, too. Females also get bladder cancer, although it’s less common.
Bladder cancer most often starts in the cells that line the inside of the bladder. It often responds well to treatment when it’s found early. Even if treatment works well, you should keep being watched for signs of bladder cancer. It can come back years later.
How common is bladder cancer?
Bladder cancer is the fifth most common kind of cancer.
- For males, it’s the fourth most common cancer.
- For females, it’s not among the top 10 most common cancers. Even so, nearly 20,000 females a year are diagnosed with bladder cancer in the United States.
Bladder Anatomy: Where is the bladder in males and females, and what does the bladder do?
The bladder is part of your urinary system. This group of organs makes urine (pee) and gets it out of your body.
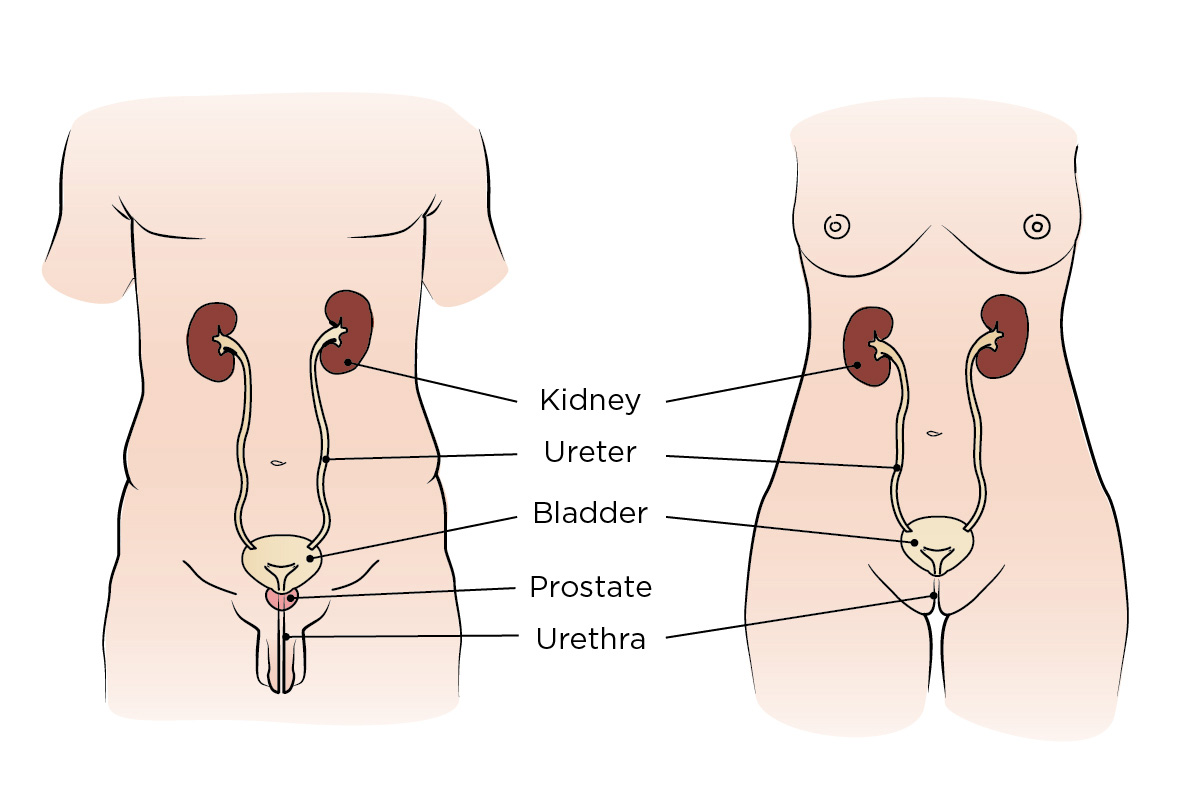
- Your bladder stores urine until you feel the need to urinate.
- Your kidneys clean the toxins out of your blood and make urine.
- Your ureters are tubes that carry urine from your kidneys to your bladder.
-
Your urethra is a tube that carries the urine in your bladder out of your body when you urinate.
- In a female body, the urethra is very short. It’s located above the vagina.
- In a male body, the tube is longer. It passes through the prostate gland and penis.
What are the types of bladder cancer?
About 9 out of 10 bladder cancers are urothelial carcinoma (also called transitional cell carcinoma). It starts in the cells on the surface of the bladder’s inner lining. Most urothelial carcinomas are non-muscle invasive bladder cancers (NMIBC). That means the cancer stays in the bladder’s inner linings.
Less common types of bladder cancer include:
- Squamous cell carcinoma
- Adenocarcinoma
- Small cell carcinoma
- Micropapillary
- Plasmacytoid
Most bladder tumors start in the inner lining and stay in the inner layers. But some bladder tumors are invasive at the time they’re diagnosed. Invasive means the cancer has spread past the layer of tissue where it started to nearby healthy tissue.
These invasive tumors can be more aggressive, which means they form, grow, or spread quickly. Invasive and noninvasive tumors have different treatments.
MSK has experts in diagnosing and treating all types of bladder cancer, including rarer forms of bladder cancers.
Learn more about the types of bladder cancer.
What are the symptoms of bladder cancer?
In most cases, an early sign of bladder cancer is painless blood in the urine (pee). This is a very common warning sign of bladder cancer for all genders.
In women, blood in the urine is often overlooked as a possible sign of bladder cancer.
The 2 most common causes of blood in the urine are a urinary tract infection (UTI) or postmenopausal uterine bleeding. Most women with blood in their urine are thought to have a UTI. As a result, women often are diagnosed with bladder cancer at a later stage, when it’s harder to treat.
Other symptoms are feeling pain or burning when you urinate. You can feel you need to urinate more often. Or, you feel like you need to urinate, but can’t. Any pain while urinating could be a sign of bladder cancer.
Signs of advanced bladder cancer include lower back pain on one side. You also can feel tired or weak. Another sign of advanced bladder cancer is having no appetite (not feeling hungry) and losing weight without trying.
All of these symptoms can be caused by something other than bladder cancer. It’s important to have them checked out by a urologist (a doctor who treats the urinary system).
Learn more about the symptoms of bladder cancer.
What are the risk factors for bladder cancer?
Smoking and tobacco use is by far the biggest risk factor for bladder cancer. People who smoke cigarettes are up to 4 times more likely than nonsmokers to get this cancer. Smoking causes about half of all bladder cancers, according to research studies. About 2 out of every 3 of people diagnosed with bladder cancer have a history of smoking.
Exposure to chemicals is another risk factor for bladder cancer. People who work in the textile, dye, rubber, leather, paint, or printing industries may also be at higher risk.
Learn more about the risk factors for bladder cancer.
How is bladder cancer diagnosed?
A common test to diagnose bladder cancer is a cystoscopy. Your doctor will put a small tube with a camera into your urethra. The urethra is the small tube that carries urine (pee) from your bladder to outside your body. Your doctor will slowly move the scope used for the cystoscopy into your bladder. They will examine the lining and take a sample.
For early-stage bladder cancer (stages 0 and 1), your doctor may be able to remove the whole tumor during the cystoscopy. This happens with urothelial bladder cancer that’s only in the inner tissues of the bladder.
Another way to diagnose bladder cancer is a urine cytology. This test analyzes a urine sample to see if it has tumor cells. Doctors also use imaging tests to look at your urinary tract.
Learn more about how bladder cancer is diagnosed.
What are the treatments for bladder cancer?
There are good treatment options for bladder cancer that’s found early. But there also are treatments that can work well for advanced bladder cancer.
Treatment aims to keep your body working as well as possible when you urinate (urinary function) and have sex (sexual function).
We may recommend some form of surgery, chemotherapy, radiation therapy, or a combination of these. For bladder cancer that grows or spreads quickly, sometimes the best treatment is removing your bladder. This is called a radical cystectomy.
When we do this surgery, we can often create a new bladder at the same time. This is called a neobladder. It lets you urinate (pee) as you normally do. You don’t need a pouch outside your body that collects urine.
Immunotherapy is a more recent way to treat bladder cancer. It uses the immune system to attack cancer cells.
We offer bacillus Calmette-Guérin (BCG) therapy. Bacillus Calmette-Guérin (buh-SIH-lus KAL-met-gay-RIN) is a type of immunotherapy used after surgery. It’s for bladder cancer that’s only in the bladder and not in the muscle. BCG treatment is an alternative to chemotherapy given inside the bladder for high grade non-muscle invasive bladder cancer (NMIBC).
People often come to MSK for BCG treatment after their healthcare provider offered chemotherapy as the only treatment option.
We use other forms of immunotherapy for people with more advanced bladder cancer. There also are promising new drugs. They include antibody-drug conjugates (ADCs), and drugs that target a certain growth pathway within cancer cells. They’re starting to change how we treat bladder cancer.
MSK also has research studies, known as clinical trials, that offer our patients new treatments often only available at MSK.
Learn more about treatments for bladder cancer.
Why should I choose Memorial Sloan Kettering for bladder cancer treatment?
MSK’s team of bladder cancer experts
MSK’s bladder cancer experts offer cancer care of the highest quality. MSK was ranked #1 in the nation for Urology Cancer Care this year by U.S. News & World Report. Our team of urinary oncology experts is among the most experienced in the field of bladder cancer. It includes world-class specialists in surgery, chemotherapy, radiation oncology, radiology, pathology, and nursing.
Our experts work very closely together. The team meets regularly to talk about people in their care and the best treatment for them. For example, our surgeons and oncologists (cancer doctors) make sure people who need chemotherapy before surgery start this treatment right away. Starting care as soon as possible may help your treatment work better.
Our bladder cancer surgeons are specialists in the most advanced ways to remove bladder tumors. Their goal is keep your body working as well as possible when you urinate (urinary function) and sexual function (having sex).
We often can successfully treat early-stage bladder cancer with minimally invasive procedures, including scopes and robot-assisted surgery. Minimally invasive surgery means it’s done with small incisions (cuts).
MSK uses the latest methods and technology to treat bladder cancer
MSK uses the latest methods available to preserve or reconstruct bladders that were partly or completely removed. We’re very experienced in bladder removal (radical cystectomy) and urinary tract reconstruction.
This includes neobladder surgery, a special procedure to create a new bladder. This approach greatly improves the quality of life for many people with bladder cancer. It often means you can avoid getting a pouch outside your body (ostomy bag or ostomy pouch) to collect urine.
MSK also offers bacillus Calmette-Guérin (BCG) therapy. It’s a type of immunotherapy we use after surgery for high grade non-muscle invasive bladder cancer (NMIBC). MSK offers BCG treatment is an alternative to chemotherapy for NMIBC.
MSK’s medical oncologists choose the best treatment for bladder cancer that have the fewest side effects. They include chemotherapy, immunotherapy, and other types of treatments.
MSK’s radiation oncologists target tumors and areas where there’s a risk the cancer can come back. Radiation oncologists are doctors who use radiation to treat cancer. At MSK, their radiation treatment is guided by very advanced imaging methods not available at most hospitals.
The MSK difference for bladder cancer
Quality of Life: People who had their bladder removed at MSK recovered well and enjoyed a high quality of life within 2 years. These excellent long-term results are from a team led by urologic surgeon Bernard Bochner. They were reported in a study published in 2022. Hundreds of MSK patients who had a radical cystectomy between 2008 and 2014 were surveyed.
People were asked about quality-of-life issues after a radical cystectomy, including:
- General quality of life
- Urinary function
- Sexual function
- Bowel function
- Body image
- Mental and emotional health
MSK patients said much of their quality of life 2 years after their surgery were the same as before their surgery. Most people said they were about back to normal within 3 months after their surgery.
Research: MSK patients have access to research studies, also known as clinical trials, that explore new and better treatments for bladder cancer. Sometimes these studies offer therapies years before they’re available anywhere else. This includes new immunotherapy methods that work very well in some people with localized or advanced bladder cancer.
Support: During and after treatment, MSK supports the physical, emotional, and spiritual needs of people with bladder cancer. MSK offers a complete program of support services. Our nurses are trained in caring for people during outpatient chemotherapy, radiation, and after surgery.
Convenient locations: You can visit MSK specialists closer to home, not just in Manhattan. We offer treatment at our regional outpatient locations in New Jersey, Westchester County, and on Long Island. You can get the same outstanding care from MSK doctors at these sites, closer to home. See all MSK locations.
Learn about our Health Information Policy.