Research done in cancer cell lines – colonies of cells that derive from a patient’s tumor and can be grown in culture indefinitely – has revealed important insights about the biology of cancer and is essential for the development of new drugs. These cell lines have been generated and shared by laboratories around the world for decades to model different types of cancer.
But scientists often question how reliable these cultured cells are as research tools. It is not always known from what subtype of cancer a particular cell line was derived or to what extent the cells actually resemble their tissue of origin after years in culture.
Now, a team of Memorial Sloan Kettering investigators has been able to examine in molecular detail the resemblance of cancer cell lines to real tumors by comparing their genomic profiles. Focusing on a common form of ovarian cancer known as high-grade serous ovarian cancer (HGSOC), the researchers found that the cell lines most often used for research are not ideal models for this disease because their genetic makeup differs significantly from that of real tumors. They reported this finding in the journal Nature Communications in July.
“A Very Useful Test Bed”
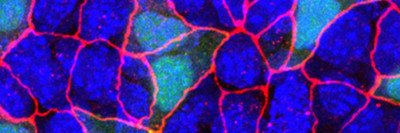
Cell models of human tumors can be generated by isolating tumor cells from a biopsy or surgery sample and growing them in culture while carefully establishing the conditions needed to make the cells thrive in a laboratory setting. The cells are then immortalized, or genetically manipulated to proliferate indefinitely. By contrast, human cells normally stop proliferating after a limited number of divisions.
Once established, a cell line can be maintained in the lab forever and used in a range of settings. For example, it can be used to investigate the basic mechanisms that drive the development and progression of a particular type of cancer, or to identify the genes and pathways that distinguish different subtypes of the disease.
In addition, “cancer cell lines are a very useful test bed for new drugs,” explains Chris Sander, Chair of the Sloan Kettering Institute’s Computational Biology Program and one of the study’s senior authors. “Before studying the therapeutic potential of a compound in animal models – and eventually in clinical trials – one often first examines its effect on cells in culture.”
In collaboration with gynecologic oncologist Douglas A. Levine, researchers are working in ovarian cancer cell lines to identify new drug combinations that could be used to control tumors that have become resistant to currently used treatments, the most common reason for treatment failure in women with this disease.
“Like many other scientists, we asked ourselves what cell lines we should use to maximize our chances of making clinically relevant discoveries,” says Nikolaus Schultz, a member of the Sander lab. “We know cells change genetically when they are immortalized and grown under laboratory conditions. Until recently, we had no way of looking at those genetic changes in detail.”
Reviewing 50 Cell Lines and Two Decades of Published Work
But researchers now have access to large sets of genome data from clinical samples investigated by The Cancer Genome Atlas (TCGA) – a nationwide project that eventually will catalogue genetic changes in more than 20 cancer types – and close to a thousand cancer cell lines that are being characterized in the Cancer Cell Line Encyclopedia (CCLE) project. Rileen Sinha, a postdoctoral researcher in the Sander lab, and Silvia Domcke, a visiting graduate student from Germany, matched data from about 50 ovarian cancer cell lines with TCGA data from more than 300 patients with the disease, and then rated the cell lines based on their genetic similarity to TCGA tumor data.
“We distinguish the ‘good, the bad and the ugly’ among cell line models of HGSOC,” they wrote in their report.
The review shows that two of the most popular lines – which together account for about 60 percent of all cell-line-based studies of ovarian cancer that have been published in the past 20 years – had relatively poor resemblance to real tumors. By contrast, 12 cell lines with the highest scores have been used in less than 1 percent of published research even though they are readily available in cell line repositories.
A Pilot for Studying Other Cancer Types
While the report does not address whether published work done in “bad” cell lines has produced misleading results, the authors were alarmed that so many studies have been done in which scientists believed they were working in HGSOC cells when, in fact, the cells had less in common with the real disease than was believed.
Their review of ovarian cancer cell lines and tumors is a pilot for future work on other tumor types. The Memorial Sloan Kettering researchers have already started to apply their method to rate cell lines representing prostate cancer, melanoma skin cancer, and glioblastoma brain tumors.
“No conclusion drawn from experiments in cell lines is necessarily valid in a clinical setting,” Dr. Sander emphasizes. “But generally speaking, by helping researchers find the cell lines that best mirror a certain subtype of cancer, both basic and preclinical research in that disease will become considerably more accurate.”