Researchers hope targeting regulatory T cells will give immunotherapy more punch against breast cancer.
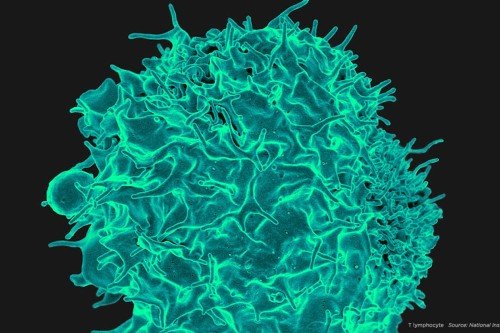
Though immunotherapy has produced impressive results against many malignancies, it has been less effective against breast cancer. Researchers think one reason for this may be the influence of a subset of immune cells called regulatory T (Treg) cells. These cells, which tamp down the immune response, are especially prevalent in breast cancer and are associated with more aggressive forms of the disease.
New research led by MSK physician-scientist George Plitas, graduate student Catherine Konopacki, and co-authors and reported in the journal Immunity suggests a promising approach for targeting these Treg cells to make breast cancer immunotherapy more potent. The strategy might make it possible to take specific Treg cells out of the equation so that other immune cells can wipe out the breast tumor.
Treg cells help rein in immune responses once they are no longer needed, preventing an attack on the body’s healthy tissues — what is called autoimmunity. Although essential to maintaining order, Treg cells also thwart the immune system from attacking tumors, which might otherwise be recognized as foreign or as different.
Researchers think tumors protect themselves from attack partly by recruiting Treg cells into their midst. Therefore, knocking out Treg cells offers a potentially effective strategy to rob cancer of this protective shield.
Dr. Plitas conducts research in the laboratory of Alexander Rudensky, Chair of the Immunology Program at the Sloan Kettering Institute and an internationally recognized leader in Treg cell research. He told us about recent progress in finding ways to get rid of specific Treg cells to help improve breast cancer responses to immunotherapy.
How does focusing on Treg cells differ from immunotherapies that have shown success in recent years?
The drugs that have worked so well against melanoma, lung cancer, kidney cancer, and bladder cancer are checkpoint inhibitors, which block receptors on the surface of a type of immune cell called effector T cells. This “releases the brakes” on these immune cells and allows them to attack anything that appears foreign. These drugs are effective because they need to inhibit just one specific immune cell pathway.
Treg cells, by contrast, appear to operate through many different pathways, meaning that they suppress the immune response through multiple mechanisms. Blocking just one of those will likely not be effective. We’ve always thought that the best way to target Treg cells is simply to get rid of them.
However, it’s very hard to target only Treg cells selectively. Some ways that have been tried were relatively nonspecific in that they took out other T cells — including effector T cells — that are needed for an immune attack. In addition, even if you target only Treg cells, you don’t want to get rid of all of them — that can cause massive autoimmunity, which is lethal.
What strategy could be used to target only certain Treg cells?
The Holy Grail is to find a way to target only those Treg cells that are in or next to tumors, while not affecting other Treg cells that are circulating in the blood. But we realized we really needed to learn more about these “tumor-resident” and “tissue-resident” Treg cells because most of what we know about human Treg cells has come from those circulating in the blood, simply because they are much more accessible.
We undertook a project to isolate human Treg cells from normal tissue, tumors, and blood and compare them. The samples were taken from our patients with breast cancer with their consent, and it required tremendous coordination with our core facilities to get them processed and analyzed. But the technology we used enables us to conduct these analyses and get answers quickly.
What did you learn about these specific Treg cells?
We found, somewhat surprisingly, that the patterns of gene expression of the Treg cells in the normal breast tissue are similar to the Treg cells in the breast tumor — but that these patterns are different from those of the Treg cells in the blood. In other words, Treg cells within a specific tissue, regardless of whether it is normal or cancerous, have their own distinct pattern.
At first, this might seem like a major problem: Any therapy aimed at cancer-specific Treg cells could cause problems in the normal tissue. However, we did see some differences between the tissue-resident and tumor-resident Treg cells. Those in the tumors had higher levels of a protein called CCR8. This suggests that targeting the CCR8 protein with an antibody could be effective in selectively depleting the tumor-resident Treg cells. Presumably, taking out these Treg cells would leave the tumor more vulnerable to attack from the other immune cells. This may represent a promising immunotherapeutic approach to treating breast cancer.
What’s the next step in translating these findings to the clinic to actually treat patients?
In our lab, we’re generating antibodies against CCR8 that could be used in clinical trials to see if we can deplete tumor-resident Treg cells. We already have some good contenders. In addition, we have found increased CCR8 expression by Treg cells from other tumor types, including lung cancer and melanoma, so it doesn’t seem to be restricted to breast cancer. I think this strategy could be broadly applicable to a number of different tumor types, used either alone or in some cases in combination with other therapies such as checkpoint blockade.
Treg cells with their multiple suppressive properties will be difficult to block. However, the cancer community believes they are a major obstacle to making immunotherapies work, particularly for cancers where responses have been limited. This is an area of research with a great amount of untapped potential.