Until recently, little was known about the underlying causes of metastasis. Yet the special abilities some tumor cells have to spread disease from a primary tumor to other organs account for nine out of ten cancer deaths.
Now opportunities to explore therapies that could limit metastasis are growing, as scientists refine their methods to observe such tumor cells traveling between organs, isolate the cells from patients or mice, and study them to learn more about the genes and proteins that make metastasis happen. “We are seeing a massive opening of the black box that contains the mechanisms of metastasis,” said Joan Massagué, who chairs the Sloan Kettering Institute’s Cancer Biology and Genetics (CBG) Program.
The Metastasis Research Center (MRC), which Dr. Massagué directs, has brought together 27 Memorial Sloan Kettering laboratories to facilitate research on metastasis and its treatment. “Those of us who work on this issue recognize that we need all the help we can get,” Dr. Massagué said. “Not only in terms of technology and resources, but also in terms of sharing our knowledge and further educating one another.
“Not many institutions in the world have the breadth of expertise, the infrastructure, and the collaborative atmosphere it takes to address broad and complicated problems,” he added. “Many times, what really moves research forward is the spontaneous interaction between scientists and clinicians. And for me, there’s no better place than Memorial Sloan Kettering for such dialogues.”
Underpinning a tumor’s spread are a myriad of biological processes, the complexity of which may account for why metastasis is so difficult to study and treat.
“The cells we are concerned with are the rarest of the rare,” Dr. Massagué noted. “But it only takes one for metastasis to occur.” In one day, millions of cells may be shed from a tumor and enter a patient’s bloodstream and lymphatic system, but only a few will survive. Fewer still will be able to force their way into a new organ, adapt to the distinct environment within it, and eventually thrive and take over.

Numerous genes are altered as a cell overcomes these hurdles. “Tumor cells are genetically unstable, and this helps them adapt to new situations,” explained Robert Benezra, of the CBG Program. “This flexibility might also help cells grow resistant to therapy over time.”
In addition, tumor cells do not act alone. “They depend on a variety of noncancerous cells in their surroundings, and on the signals these cells send out,” said Johanna Joyce, of the CBG Program. “Tumor cells can hijack normal cells that are present in a primary tumor or at a metastatic site and use them to their own advantage.”
To make things even more complicated, each cancer is unique. Not only do different tumor types spread to different organs — for instance, colorectal tumors often target the liver and lungs, while prostate tumors usually spread to the bone — the pace of metastasis varies too. “Both breast and lung cancers can target the brain, bone, and liver,” Dr. Massagué explained. “But while lung cancer spreads rapidly, often within months after a patient has been diagnosed, disseminated breast cancer cells can take many years to form metastases.”
He and his colleagues are discovering the genes that give tumor cells the specialized traits they need to infiltrate their target organs, survive in them, and spawn new tumors. For example, experiments in mouse models and patient-derived tumor cells, and analyses of large clinical datasets, have recently allowed the investigators to identify three genes that breast tumor cells use to cross the blood-brain barrier — a network of capillaries that is impenetrable to most blood-borne cells — and enter the brain.
Another study showed that the activation of a gene product called SRC helps breast cancer cells to enter bone marrow and reside there latently, sometimes for decades. The presence of such cells might explain why certain patients, in spite of showing no signs of disease, relapse with bone metastases many years after treatment. “We are now designing clinical trials to find and analyze such cells, and attack them with a drug that inhibits SRC,” said Larry Norton, Memorial Hospital’s Deputy Physician-in-Chief for Breast Cancer Programs, who participated in the study.
Using mathematical modeling approaches, Dr. Norton and colleagues are also devising therapeutic strategies that could prevent a patient’s circulating tumor cells from revitalizing the tumor they once detached from — a newly discovered phenomenon called self-seeding — as well as from seeding new tumors around the patient’s body.
“All of us within the MRC look at metastasis with different eyes,” said Filippo Giancotti. His lab, in SKI’s Cell Biology Program, is investigating how signals that tumor cells receive from their surroundings can spur a cancer’s progression.
For example, the investigators are studying receptors called integrins, which are known to mediate a cell’s attachment to the extracellular matrix — a structure that holds the cells within a tissue together. Their research indicates that cells within a primary tumor also use the receptors to detach from other cells, and to migrate away from the tumor mass toward nearby blood vessels.
In addition, Dr. Giancotti and his co-workers are investigating tumor dormancy, a poorly understood phenomenon that is an emerging area of research. Upon entering a new tissue, some disseminated tumor cells stop dividing and do not cause symptoms until they are induced to exit from their dormant state.
“If we understood what enables these cells to remain dormant for a long period, and what signals awaken them, it might be possible to prevent metastatic tumor growth pharmacologically,” Dr. Giancotti added.
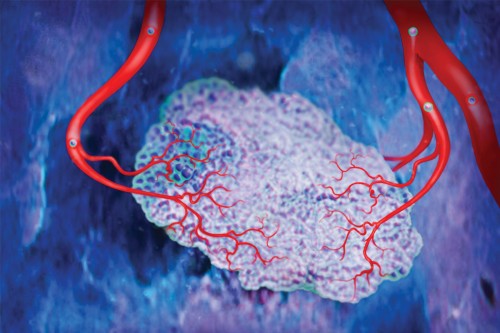
Researchers are also learning how tumor cells tap into the genetic programs that guide embryonic development. “A tumor is a bit like an embryo,” said Dr. Benezra. “It invades new tissues and acquires new blood vessels in ways that are similar to how an embryo establishes itself in the maternal uterus.”
His lab investigates a set of genes called Id, which normally are active only during embryonic development. By reactivating the genes, a tumor can induce the formation and growth of blood vessels in its surrounding vasculature, a process known as angiogenesis, to gain more blood supply — and new avenues through which cells can travel.
Dr. Benezra and his colleagues have developed a compound to target the activity of Id genes, which in preclinical testing was shown to reduce tumor-induced angiogenesis and metastasis. “We hope it can offer a powerful antimetastatic strategy for the clinic,” he said.

In Dr. Joyce’s lab, research is focused on how tumor cells interact with their microenvironment — the network of noncancerous cells with which they coexist — and how this communication could be exploited therapeutically.
For example, white blood cells called macrophages are recruited from the bone marrow to a primary tumor by signals that tumor cells emit. Dr. Joyce’s lab has shown that such macrophages “are tricked by tumor cells into secreting protein-degrading enzymes called cathepsins,” she explained. By dissolving the extracellular matrix surrounding the tumor, macrophages help create the paths for tumor cells to escape and invade blood vessels.
Dr. Joyce and her colleagues have been able to hamper the ability of tumor cells to invade the blood circulation in mice using small molecules that block the activity of cathepsins. “In the future, cathepsin inhibitors might be used to target a patient’s tumor-associated macrophages, likely in combination with therapies directed against tumor cells,” she said.
And there are other reasons why prospective therapies might be designed to attack both tumor cells and normal cells — or, as Katrina Podsypanina put it, “tumor cells and their unfortunate neighbors, which appear to be normal,” though these neighboring cells may in fact be corrupted by cancer or its treatment.
Dr. Podsypanina and Nancy Du are research fellows in the laboratory of Memorial Sloan Kettering President Harold Varmus, who is also a member of SKI’s CBG Program. They are examining the conditions under which metastasis occurs using mouse breast tumor models in which oncogenes can be turned on and off artificially. (Oncogenes are genes that, when altered by mutation or overly activated, make cells cancerous.)
“Our research shows that a mouse’s normal breast cells, in which no oncogenes are active, can seed in the lung if we inject them into the bloodstream,” Dr. Podsypanina explained. Once seeded, the breast cells can reside in the lung and grow new tumors eventually, if oncogenes are activated. The findings have alerted the investigators to the possibility that cells in a tumor’s proximity, which are not yet cancerous, could instigate metastasis.
“We don’t know under what conditions normal cells can enter the bloodstream, allowing them to disseminate and seed in new organs, if they do it at all, or what effect that could have on the patient’s disease,” she added. “But it’s something we plan to investigate. Given that most therapies were designed to target cancer cells only, sparing normal cells, there might be reasons to rethink our strategies.”
Going forward, Dr. Massagué says his lab and others within the MRC will extend their efforts into areas where metastasis research is especially urgent. “For example, metastasis to the brain is a terrible condition and has been very challenging to study,” he noted. In the United States alone, approximately 170,000 people are affected by brain metastasis each year, mainly from breast and lung cancer.
Last year, Dr. Massagué and colleagues uncovered mechanisms that cause the swift spread of lung cancer to the brain and bone. “Lung cancer is one of many deadly cancers whose metastasis processes have not received the attention they deserve,” he said, adding that research has a tendency to prevail in diseases for which funding, clinical samples, and experimental models are at hand. “We aim to focus on the cancers in which progress is needed most,” he said, “and, hopefully, we’ll inspire more labs around the world to join the effort.”
Additional Information
See all extras related to this article.
more