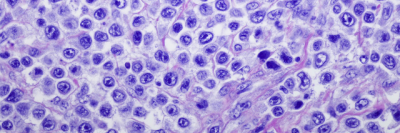
Non-Hodgkin lymphoma (NHL) is the most common type of lymphoma. While it can occur at any age, most people who develop the illness are older adults.
Read more about lymphoma in children or about Hodgkin lymphoma.
There are many types of NHL, all of which are divided into two major groups: B cell lymphoma and T cell lymphoma.
Types of B cell lymphoma
B cell lymphoma is much more common. It accounts for about 80 percent of all NHL cases. It includes:
- diffuse large B-cell lymphoma
- primary mediastinal B cell lymphoma
- follicular lymphoma
- small lymphocytic lymphoma and chronic lymphocytic leukemia
- marginal zone lymphoma
- mantle cell lymphoma
- Waldenström’s macroglobulinemia
- Burkitt lymphoma
Types of T cell lymphoma
T cell lymphoma accounts for approximately 15 percent of all cases of NHL in the United States. The most common types of T cell lymphoma include:
- peripheral T cell lymphoma not otherwise specified
- anaplastic large cell lymphoma
- angioimmunoblastic lymphoma
- cutaneous T cell lymphoma
There are also several types of relatively rare T cell non-Hodgkin lymphoma.
Request an Appointment
Call 646-497-9137
We’re available 24 hours a day, 7 days a week
We’re available 24 hours a day, 7 days a week