At the annual San Antonio Breast Cancer Symposium, MSK investigators presented the latest research on detection and screening methods for people at high risk; immunotherapy for breast cancer; and the underlying causes of resistance to targeted therapies, among other topics.
Here are some of the noteworthy studies that featured contributions from MSK investigators.
Rethinking Imaging Approaches for High-Risk Women
Mammography screening has been shown to reduce breast cancer mortality by about 30% in the general population. But in women at an increased risk for the disease, additional imaging is recommended. This group includes people who carry a BRCA or other genetic mutation. Other risk factors include a family or personal history of breast cancer, certain high-risk lesions, or having undergone chest radiation at a young age.
At SABCS, diagnostic radiologist Maxine Jochelson discussed newer imaging technologies and the advantages they have over mammograms alone for detecting cancer in high-risk women. “People in the high-risk group may need supplemental imaging to improve early detection,” Dr. Jochelson says.
She explains that this approach would incorporate vascular imaging techniques. These methods can highlight areas of increased blood flow, a hallmark of tumor growth. This technology includes MRI and contrast-enhanced mammography. It can find tumors that mammograms may miss. Although vascular imaging costs more and generally takes longer to perform, its use is justified in high-risk women because of the increased chance of finding cancer, she says.
“It’s undisputed that vascular imaging is better at detecting cancers than purely anatomical imaging,” Dr. Jochelson adds. She emphasizes the need to fine-tune imaging strategies based on each person’s specific risk factors.
Some of the imaging approaches she discussed during her presentation include:
- improved anatomic imaging techniques, such as whole-breast ultrasound and digital breast tomosynthesis, which creates a 3-D picture of the breast using X-rays
- vascular imaging methods, such as contrast-enhanced digital mammography, which is cheaper and quicker than MRI
- abbreviated breast MRI, which involves taking fewer images than conventional MRI and having them interpreted faster
“We need to continue improving ways of assessing an individual’s risk so we can stratify them and determine which type of imaging will most benefit each patient,” Dr. Jochelson says. “The true test will be studies to demonstrate that these newer technologies actually save lives.”
A New Approach for Treating Breast Cancer with Immunotherapy
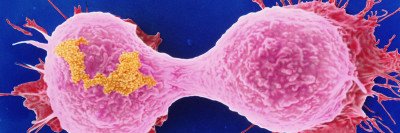
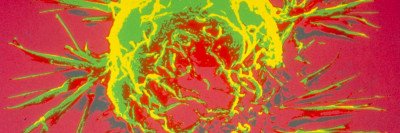
Immunotherapy that uses genetically engineered cells, such as chimeric antigen receptor (CAR) T cells, has proven effective in treating some forms of blood cancer. So far, efforts to create immune cells that can effectively target solid tumors, including breast cancer, have been disappointing. At SABCS, MSK physician-scientist Christopher Klebanoff presented research from his lab on a novel tactic for enabling the immune system to better target and kill breast cancer cells while sparing healthy tissue.
“We believe a major limiting challenge in successfully developing immunotherapy for breast cancer has been the identification of antigens. These are targets that the immune system can recognize,” Dr. Klebanoff explains. “We’ve become very interested in the possibility that common mutations in breast cancer may produce antigens that can be recognized as foreign by the immune system.”
The Klebanoff lab’s current research focuses on a gene called PIK3CA, which is mutated in about 40 to 45% of hormone receptor-positive breast cancers. It is also mutated in some HER2-positive and triple-negative breast cancers. Mutations in PIK3CA cause cancer cells to grow in an uncontrolled manner. In May 2019, the US Food and Drug Administration approved a pill called alpelisib (Piqray®), which targets mutations in this gene. However, the drug has the potential for significant side effects, and tumors ultimately develop resistance to this medicine. Dr. Klebanoff and his colleague Smita Chandran, a senior research scientist in his lab and the scientific lead on this study, decided to look for a way to target antigens created by this mutation using immune cells designed to recognize them.
A challenging aspect of this approach was that mutated PIK3CA is found on the inside of cancer cells, allowing it to hide from many components of the immune system, such as antibodies. “Physiological processes present in all cells, including cancer cells, allow mutated PIK3CA to be broken down into shorter fragments and loaded onto a molecular ‘basket,’ called HLA, which is shuttled to the surface of the cell,” Dr. Klebanoff says. “This process allows immune cells to functionally look inside of other cells.”
The researchers identified a specialized molecule, known as a T cell receptor, that has the ability to recognize this mutated PIK3CA-HLA complex. Immune cells specific for this complex recognize the target cell as being cancerous and destroy it. Healthy cells without the mutation remain untouched. The T cell receptors are matched to a patient’s unique complement of HLA molecules. As with a stem cell transplant, HLA must be matched for this immunotherapy to be effective.
“Right now we are focused on the most common HLA types that are seen in a large proportion of our patients. The big-picture goal is to build a library of T cell receptors that can work in people with different HLA molecules and can target other common cancer mutations,” Dr. Chandran explains. “This work is still early and so far has only been done in the laboratory and not in humans. We are nonetheless excited about the prospect of working toward developing a more effective and less toxic immunotherapy customized to the genetic attributes of a patient’s tumor.”
Understanding Resistance in ER-Positive Disease
CDK4/6 inhibitors are an important class of drugs to treat estrogen receptor-positive breast cancer. These drugs stop the growth of breast cancer cells by targeting enzymes that are important in cell division. They are given in addition to hormone therapy. But about 10 to 15% of people who get these drugs don’t respond to CDK4/6 inhibitors, and others later develop resistance.
MSK physician-scientist Sarat Chandarlapaty has been studying why this is the case. Understanding this resistance could contribute to the development of new targeted drugs. In December 2018, he published a study that reported on two genes that play a critical role in promoting this resistance. At SABCS, he presented his latest research on this area.
“We’ve been delving deeper into the role of these genes, as well as others, to try to understand some of the principles that could guide the next generation of therapies,” Dr. Chandarlapaty says. “By working out these detailed mechanisms, we will have the tools needed to design more potent and selective inhibitors for these refractory breast cancers.”
Dr. Chandarlapaty explains that because tumors outsmart CDK4/6 inhibitors in different ways, he doesn’t expect to find a one-size-fits-all approach for new drugs. “There are some key principles for why these drugs fail,” he says. “For some tumors, making a more potent drug of the same general class will work. Other tumors bypass the pathway in a way that renders many of the old therapies we’ve used ineffective. For them, a completely different approach is needed.”