This information will help you get ready for your cystoscopy (sis-TOS-koh-pee) and related procedures at MSK. It describes cystoscopies done in the operating room.
About your cystoscopy
Cystoscopy is a procedure that lets your healthcare provider look for problems in your urinary tract and bladder. This includes a blockage in your urethra or tumors in your bladder.
A surgical urologist will do your cystoscopy. A urologist is a doctor with special training in the genitourinary (jeh-nih-toh-YOOR-ih-nayr-ee) system. The genitourinary (GU) system includes the bladder, kidney, penis, prostate, and testicles.
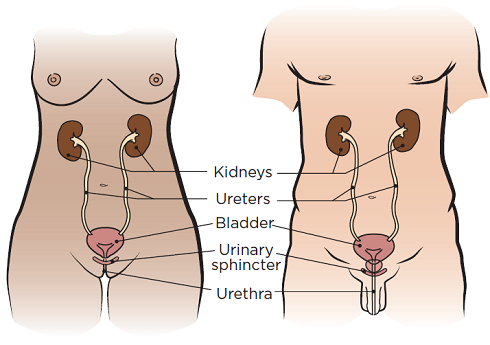
Your urologist will use a cystoscope to look at your urethra, bladder, and the openings to your ureters. A cystoscope is thin, hollow tool with a light on the end. Your ureters are the tubes that carry urine (pee) from your kidneys to your bladder (see Figure 1).
During your cystoscopy, your urologist will put the cystoscope into your urethra and slowly move it into your bladder. They can put small surgical tools through the cystoscope to remove stones, fulgurate (burn off) small growths. They may also do a biopsy to find out if the tumors have spread to your lymph nodes. This means they will take a small tissue sample to look at it more closely.
Other procedures
You may also have 1 or more of the following procedures during your cystoscopy.
Transurethral resection of a bladder tumor (TURBT)
During a TURBT, your healthcare provider will remove a bladder tumor using a tool that goes through the cystoscope.
Ureteroscopy
During a ureteroscopy (YER-eh-ter-OS-koh-pee), your healthcare provider will put a thin tool called a ureteroscope through your urethra, bladder, and ureter. This procedure is done to see if there’s anything blocking or getting in the way of the flow of urine.
Retrograde pyelogram
During a retrograde pyelogram (REH-troh-grayd PY-eh-loh-gram), your healthcare provider will guide catheters to your kidneys through your ureters. Catheters are thin, flexible tubes.
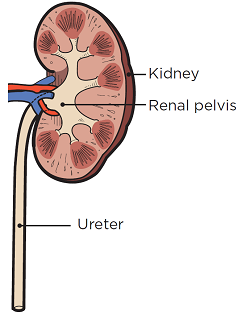
Your healthcare provider will inject contrast through the catheters into your kidneys. Contrast is a special dye that helps make the images from your X-rays clearer. Then, they’ll take X-rays of your renal pelvis and ureters (see Figure 2). This procedure is done to see if there’s anything blocking or getting in the way of the flow of your urine.
Placement, replacement, or removal of ureteral stents
The stents will keep your ureters open. That helps urine flow from your kidneys to your bladder. If your kidney function has improved, your healthcare provider may decide to remove the stent(s) and you may not need a replacement.
Botox bladder injections
During a Botox bladder injection (shot), your healthcare provider will use a needle to inject Botox into your bladder. Botox is a drug used medically to treat muscle problems that lead to spasms. The Botox injection will help reduce bladder spasms and incontinence. Incontinence is leakage of urine (pee) or stool (poop) that you cannot control.
Removal of stones or blood clots from your bladder
What to do before your procedure
Ask about your medicines
Tell your healthcare provider what medicines you’re taking, including prescription and over-the counter medicines, patches, creams, and herbal supplements. You may need to stop taking some of them before your procedure.
If you take medicine to thin your blood, ask the healthcare provider who prescribes it for you when to stop taking it. Blood thinners are used to treat blood clots or to prevent a heart attack or stroke. Examples include:
- aspirin
- warfarin (Coumadin®)
- dalteparin (Fragmin®)
- heparin
- tinzaparin (Innohep®)
- enoxaparin (Lovenox®)
- clopidogrel (Plavix®)
- cilostazol (Pletal®)
- dabigatran (Pradaxa®)
- apixaban (Eliquis®)
Tell your healthcare provider if you’ve had an allergic reaction to contrast media in the past.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
What to do 7 days before your procedure
Follow your healthcare provider’s instructions for taking aspirin
Aspirin can cause bleeding. If you take aspirin or a medicine that has aspirin, you may need to change your dose or stop taking it 7 days before your procedure. Follow your healthcare provider’s instructions. Do not stop taking aspirin unless they tell you to.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
Stop taking vitamin E, multivitamins, herbal remedies, and other dietary supplements
Vitamin E, multivitamins, herbal remedies, and other dietary supplements can cause bleeding. Stop taking them 7 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read Herbal Remedies and Cancer Treatment.
What to do 2 days before your procedure
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
What to do the day before your procedure
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-7606.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
This will be one of the following locations:
-
Presurgical Center (PSC) on the 2nd Floor
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
M elevator to the 2nd floor -
Presurgical Center (PSC) on the 6th Floor
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
B elevator to the 6th floor
Visit www.msk.org/parking for parking information and directions to all MSK locations.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your procedure. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their procedure.
What to do the day of your procedure
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before procedures, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your procedure.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Things to remember
- Take a shower with soap and water. You can brush your teeth and rinse your mouth.
- Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne.
- Do not wear any metal objects. Take off all jewelry, including body piercings.
- Leave valuable items (such as credit cards, jewelry, and your checkbook) at home.
- Bring only the money you may want for small purchases (such as a newspaper).
What to expect when you arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having a procedure on the same day. Once you’re in the department, you’ll fill out a brief questionnaire
When it’s time for your procedure, you’ll remove your hearing aids, glasses, and dentures, if you have them. You’ll either walk into the procedure room or a staff member will bring you there on a stretcher.
Your nurse will place an intravenous (IV) line in your vein. The IV line will be used to give you anesthesia (medicine to make you sleep) before and during your procedure.
Once you’re asleep, your healthcare provider will do the cystoscopy and any other procedures you’re having. They may put a urinary (Foley) catheter into your bladder at the end of your cystoscopy to help drain your urine into a bag.
Your procedure will take up to 1 hour.
What to do after your procedure
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your procedure. A nurse will keep track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You may have compression boots on your lower legs.
You may also have a urinary (Foley) catheter in your bladder to make sure your bladder is emptying. If you do, your nurse will remove it before you go home to see if you can empty your bladder. If you can’t, you’ll go home with the catheter in for few more days. Your nurse will show you how to care for it before you go home. They will tell you when they will remove the catheter and explain your discharge instructions to you and your caregiver.
At home
- You may need to take medicine at home, such as antibiotics to prevent infection or medicine to relieve discomfort. Follow the instructions your healthcare provider gives you.
- Do not drive for 24 hours after your procedure.
- Ask your healthcare provider when you can go back to work.
- Drink 8 (8-ounce) cups of liquids every day for the first 2 weeks after your procedure. Avoid drinking liquids after 8 p.m. so you do not have to go to the bathroom during the night.
- Be sure to get plenty of rest.
Changes when you urinate
You’ll most likely have hematuria (blood in your urine) after your procedure. This should go away within 1 week.
You may also urinate more often than usual and have pain or burning when you urinate. These symptoms can last for 3 to 4 weeks, but they should slowly get better as you heal. Drinking lots of liquids will also help.
Call your healthcare provider if these changes do not get better or if they get worse. You may have a urinary tract infection (UTI).
Urinary catheter
You may feel a strong urge to urinate while the catheter is in place. This happens because the small, inflated balloon that keeps it in place may make your bladder feel full. Relaxing and letting the urine flow will decrease this urge.
Biopsy or tumor removal
If you had a biopsy or a tumor removal, you’ll have a scab inside your bladder. The scab will loosen within a month. If it loosens before the wound is completely healed, it may cause bleeding. If this happens, rest and drink more liquids.
Most bleeding will stop within 3 to 4 hours, but it’s best to rest that day to help stop the bleeding. Call your healthcare provider if the bleeding doesn’t stop or if you cannot urinate.
Urinary stents
You may feel the stents. They usually feel like pain in your kidney (your side or middle to upper back). The pain may be worse when you urinate or exercise. Your healthcare provider may give you medicine to help with the pain. Drink plenty of liquids while you have the stents.
Activity
- If you need to go on car trips that are longer than 1 hour for 1 week after your procedure, talk with your healthcare provider.
- Do not lift objects heavier than 10 pounds (4.5 kilograms) for 2 weeks after your procedure.
- Do not do strenuous exercise, such as tennis, jogging, or exercise programs, for 2 weeks after your procedure.
- You can walk and climb stairs right away after your procedure.
Follow-up care
If you had ureteral stents placed during your procedure, call your healthcare provider’s office to schedule a follow-up appointment. The stents will need to be changed every 3 to 6 months, or as instructed by your healthcare provider.
When to call your healthcare provider
Call your healthcare provider if you have:
- Continuous bright red blood or blood clots in your urine.
- Bleeding (pink urine) for more than 1 week that isn’t getting better.
- Pain or burning when you urinate for more than 3 days that isn’t getting better.
- Frequent urination for more than 3 days that isn’t getting better.
- A fever of 101 °F (38.3 °C) or higher.
- Shaking chills.
- Pain in your lower back.
- An inability to urinate.
