This information will help you get ready for your transrectal prostate biopsy with ultrasound under anesthesia. Anesthesia is medicine to make you sleep during a procedure. It will also explain what to expect after your biopsy.
About your prostate
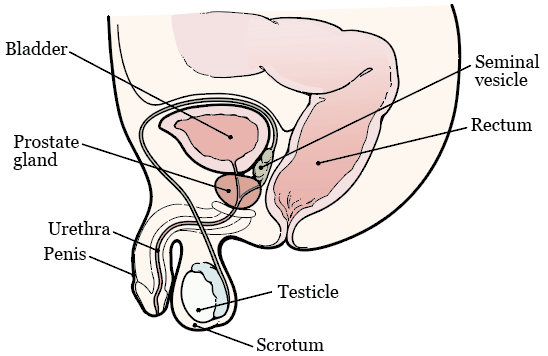
Your prostate is a small, firm gland about the size of a walnut. It’s in front of your rectum, below your bladder (see Figure 1). Your prostate works with other glands in your body to make semen. It surrounds your urethra, the tube that drains urine (pee) from your bladder.
About your prostate biopsy with ultrasound
A prostate biopsy is a procedure to collect small pieces of tissue from your prostate. An ultrasound is an imaging scan that uses sound waves to make pictures of the inside of your body.
Your healthcare provider will use ultrasound imaging during your biopsy. This will help them take tissue from the right areas of your prostate. After your biopsy, they will use a microscope to check the tissue for cells that are not normal.
Getting ready for your prostate biopsy
Talk with your healthcare provider
Tell your healthcare provider if you take anticoagulants (blood thinners). These are medicines that affect the way your blood clots.
We’ve listed some examples of common blood thinners below. There are others, so be sure your care team knows all the medicines you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Also tell your healthcare provider if you:
- Take steroids, such as prednisone (Deltasone®).
- Have taken any antibiotics in the past 3 months.
- Take any other medicine, including vitamin E, multivitamins, herbal remedies, or any other dietary supplements or home remedies. Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil. It has information about medicines you’ll need to avoid before your procedure.
Buy your supplies
Buy the following supplies before your biopsy.
- 1 saline enema, such as a Fleet® saline enema. You can buy this at your local pharmacy without a prescription.
- Oral antibiotic (antibiotic that you swallow), if your healthcare provider tells you to. If you’re taking an oral antibiotic, your healthcare provider will give you a prescription. Read the “Oral antibiotics” section for more information.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
What to do 7 days before your prostate biopsy
Stop taking certain medicine
You may need to stop taking some of your medications before your biopsy. Examples include anticoagulants, aspirin, medications that contain aspirin, multivitamins, and vitamin E. Talk with your healthcare provider about which medications are safe for you to stop taking. Follow their instructions.
Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil to learn more.
Weight loss medicines
If you take medicine for weight loss (such as a GLP-1 medicine), talk with the healthcare provider doing your procedure. Ask them what to do before your procedure. You may need to stop taking it, follow different eating and drinking instructions before your procedure, or both. Follow your healthcare provider’s instructions.
We’ve listed some examples of medicines that cause weight loss below. There are others, so be sure your care team knows all the medicines you take. Some of these are meant to be used to help manage diabetes but are sometimes prescribed just for weight loss.
|
|
What to do 2 days before your prostate biopsy
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
What to do the day before your prostate biopsy
A staff member from the Admitting Office will call you after 2 p.m. the day before your biopsy. If your biopsy is scheduled for a Monday, they’ll call you the Friday before. If you don’t get a call by , call 212-639-5014.
The staff member will tell you what time to get to the hospital for your biopsy. They’ll also remind you where to go. This will be one of these locations:
Presurgical Center (PSC) on the 2nd floor
1275 York Ave. (between East 67th and East 68th streets)
M Elevator to 2nd Floor
Presurgical Center (PSC) on the 6th floor
1275 York Ave. (between East 67th and East 68th streets)
B elevator to 6th Floor
Josie Robertson procedure Center (JRSC)
1133 York Ave. (between East 61st and East 62nd streets)
If you have any changes in your health or need to cancel your biopsy for any reason, call your surgeon. Offices are usually open Monday through Friday from 9 a.m. to 5 p.m. After , during the weekend, and on holidays, call 212-639-2000. Ask for the doctor who is covering for your doctor.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your procedure. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their procedure.
What to do the day of your prostate biopsy
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before procedures, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your procedure.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Give yourself a saline enema
Give yourself a saline enema the morning of your biopsy. Follow the directions on the box.
Take your antibiotics
You will need to take an antibiotic to prevent infection from the biopsy. Your healthcare provider will tell you which antibiotic you’ll take. They will also give you a prescription for one of the antibiotics listed below.
-
Ciprofloxacin (Cipro®) 500 mg (2 tablets)
- Take 1 tablet 2 hours before your biopsy.
- Take 1 tablet 12 hours later.
-
Cefixime (Suprax®) 400 mg (1 tablet)
- Take 1 tablet 2 hours before your biopsy.
-
Cefuroxime (Ceftin®) 500 mg (2 tablets)
- Take 1 tablet 2 hours before your biopsy.
- Take 1 tablet 12 hours later.
-
Sulfamethoxazole-trimethoprim (Bactrim®) 500mg (2 tablets)
- Take 1 tablet 2 hours before your biopsy.
- Take 1 tablet 12 hours later.
Intravenous (IV) antibiotics
Your healthcare provider might decide you need IV antibiotics instead of oral antibiotics. If they do, they will give it to you through a vein in your arm while you’re in the hospital.
Things to remember
- Do not wear any metal objects. Take off all jewelry, including body piercings. The equipment used during your biopsy can cause burns if it touches metal.
- Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne.
- Leave valuable items, such as credit cards, jewelry, and your checkbook, at home.
- If you wear contact lenses, wear your glasses instead. Wearing contact lenses during a procedure can damage your eyes. Remember to bring a case for them.
What to expect when you arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having a procedure on the same day.
You may need to fill out a brief questionnaire if you have not already done so through MSK MyChart, the patient portal.
We’ll give you a hospital gown, robe, and nonskid socks to wear when it’s time to change for your procedure.
Get ready for your procedure
When it’s time for your procedure, you’ll take off your eyeglasses, hearing aids, dentures, prosthetic devices, wig, and religious articles.
You’ll go into the procedure room. A member of the procedure room team will help you onto the procedure bed.
The exact starting time of your biopsy may depend on the length of the procedure scheduled before yours. Your nurse will speak with you if there are any unexpected delays.
Your biopsy will take about 20 to 30 minutes.
What to do after your prostate biopsy
After your biopsy, you will need to urinate before you leave the hospital.
It’s normal to have some soreness or discomfort after your biopsy, but most people don’t have pain. If you feel sore, you can take acetaminophen (Tylenol®). If the acetaminophen doesn’t help, call your doctor’s office.
For 3 days after your biopsy, try to drink double the amount of liquids you usually drink. This will help flush out your bladder, prevent infection, and minimize the amount of blood in your urine. It will also help soften your bowel movements (poop), which helps keep your rectum from getting irritated.
Filling out your recovery tracker
We want to know how you’re feeling after you leave the hospital. To help us care for you, we’ll send questions to your MSK MyChart account. We’ll send them every day for 5 days after you’re discharged. These questions are known as your Recovery Tracker.
Fill out your Recovery Tracker every day before midnight (12 a.m.). It only takes 2 to 3 minutes to complete. Your answers to these questions will help us understand how you’re feeling and what you need.
Based on your answers, we may reach out to you for more information. Sometimes, we may ask you to call your surgeon’s office. You can always contact your surgeon’s office if you have any questions.
Read Common Questions About MSK's Recovery Tracker to learn more.
Short-term effects of your biopsy
Bowel movements
You might see blood in your bowel movements. You might also have a small amount of bleeding from your rectum. These can happen right after your biopsy or for the next few days when you have a bowel movement.
Urine
You might see blood in your urine for 1 to 2 weeks after your biopsy. This bleeding might come and go.
Semen
Your semen might look rust-colored for up to 12 weeks after your biopsy. This is because small amounts of blood might be in it.
Activities after your biopsy
Tell your nurse if you’ll be more than 2 hours away from MSK during the first 24 hours after your biopsy. You might have to go to MSK’s Urgent Care Center (UCC) if you have any problems after your biopsy. This includes fever or bleeding.
Don’t have sex for 3 days after your biopsy.
For the next 5 days after your biopsy, do not:
- Play any sports.
- Work out in a gym.
- Ride a bicycle.
- Lift any objects heavier than 10 pounds (4.5 kilograms).
Getting your test results
Your test results will be ready 5 to 7 days after your biopsy. Your healthcare provider will contact you and explain the results to you. You can also ask for a copy of your results.
When to call your healthcare provider
Call your healthcare provider right away if you have:
- A fever of 101 °F (38.3 °C) or higher.
- Heavy bleeding from your rectum.
- Bleeding from your rectum that will not stop.
- You can’t urinate.
- Bright red blood or large clots in your urine.
- Shaking chills.
- Dizziness.
- Any other problems, questions, or concerns.