This excerpt from About Your Thoracic Surgery describes what to expect after your thoracic surgery at MSK.
Write down any questions you have and be sure to ask your healthcare provider.
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your surgery. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
You may stay in the PACU for a few hours or overnight.
Tubes and Drains After Thoracic Surgery
You will have the following tubes and drains. Your healthcare provider will talk with you about what to expect.
- A urinary (Foley) catheter: This is a tube that drains urine from your bladder. Your care team will keep track of how much urine you’re making while you’re in the hospital.
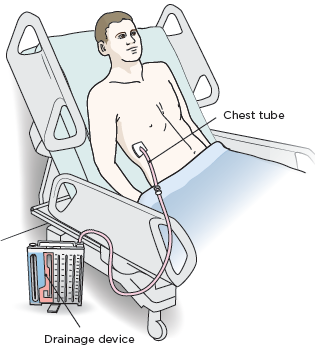
- A chest tube: This is a tube that drains blood, fluid, and air from around your lung. The tube is placed between your ribs and goes into the space between your chest wall and lung (see Figure 1). Your care team will keep track of how much drainage you have. Your chest tube will be removed when your lung is no longer leaking air. Most people go home the same day that their chest tube is removed
- Drainage device: This device is attached to your chest tube. This is where the blood, fluid, and air drained from around your lung will go.
How to Recover from Thoracic Surgery in Your Hospital Room
After you stay in the PACU, you will be taken to your hospital room. In your hospital room, you will meet one of the nurses who will care for you during your stay. Soon after you get there, a nurse will help you out of bed and into your chair.
Tell the nurse if you drink alcohol every day or if you have recently stopped drinking alcohol. Tell the nurse if you smoke or if you have recently quit smoking. They will offer you nicotine replacement therapy to make you more comfortable while you’re in the hospital.
Your healthcare providers will teach you how to care for yourself while you’re recovering from your surgery.
You can help yourself recover more quickly after thoracic surgery by:
- Reading your recovery pathway. Your healthcare provider will give you a pathway with goals for your recovery if you do not already have one. It will help you know what to do and expect on each day during your recovery.
- Starting to move around as soon as you can. The sooner you get out of bed and walk, the quicker you can get back to your normal activities. Walking every 2 hours is a good goal. This will help prevent blood clots in your legs and lower your risk of developing pneumonia. You will have tubes and an IV line, so make sure you have help while you’re walking.
- Use your incentive spirometer. This will help your lungs expand, which prevents pneumonia. For more information, read our resource How To Use Your Incentive Spirometer.
- Do your breathing and coughing exercises. Practice taking deep breaths and coughing every hour while you’re awake.
Managing Pain After Thoracic Surgery
You will have some pain after your thoracic surgery. At first, you’ll get your pain medication through your epidural catheter or IV line. You’ll be able to control your pain medication using a PCA device. Once your epidural catheter or IV line is removed, your care team will teach you how to give yourself pain medication through your feeding tube.
Your healthcare providers will ask you about your pain often and give you medication as needed. If your pain is not relieved, tell one of your healthcare providers. It’s important to control your pain so you can use your incentive spirometer and move around. Controlling your pain will help you recover better.
You’ll get a prescription for pain medication before you leave the hospital. Talk with your healthcare provider about possible side effects and when to start switching to over-the-counter pain medications.
Moving around and walking
Moving around and walking will help lower your risk for blood clots and pneumonia (lung infection). It will also help you start passing gas and having bowel movements (pooping) again. Your nurse, physical therapist, or occupational therapist will help you move around, if needed.
To learn more about how walking can help you recover, read Frequently Asked Questions About Walking After Your Surgery.
To learn what you can do to stay safe and keep from falling while you’re in the hospital, read Call! Don't Fall!.
Eating and Drinking After Thoracic Surgery
You’ll slowly go back to eating solid foods starting the day after your thoracic surgery. Read your pathway and talk with your care team for more information.
If you have questions about your diet, ask to see a clinical dietitian nutritionist.
Leaving the Hospital
- On the day of your discharge, plan to leave the hospital around 11 a.m. Before you leave, your healthcare provider will write your discharge order and prescriptions. You’ll also get written discharge instructions. One of your healthcare providers will review them with you before you leave.
-
Your doctor will talk with you if you need to stay in the hospital longer than planned. Examples of things that can cause you to stay in the hospital longer include:
- Air leaking from your lung.
- Having an irregular heart rate.
- Having problems with your breathing.
- Having a fever of 101 °F (38.3 °C) or higher.
How to Recover from Thoracic Surgery at Home
Read What You Can Do to Avoid Falling to learn what you can do to stay safe and keep from falling.
Filling Out Your Recovery Tracker
We want to know how you’re feeling after you leave the hospital. To help us care for you, we’ll send questions to your MSK MyChart account. We’ll send them every day for 10 days after you’re discharged. These questions are known as your Recovery Tracker.
Fill out your Recovery Tracker every day before midnight (12 a.m.). It only takes 2 to 3 minutes to complete. Your answers to these questions will help us understand how you’re feeling and what you need.
Based on your answers, we may reach out to you for more information. Sometimes, we may ask you to call your surgeon’s office. You can always contact your surgeon’s office if you have any questions.
To learn more, read Common Questions About MSK's Recovery Tracker.
Using MSK MyChart
MSK MyChart (mskmychart.mskcc.org) is MSK’s patient portal. You can use it to send and read messages from your care team, view your test results, see your appointment dates and times, and more. You can also invite your caregiver to make their own account so they can see information about your care.
If you do not have an MSK MyChart account, you can sign up at mskmychart.mskcc.org. You can also ask a member of your care team to send you an invitation.
If you need help with your account, call the MSK MyChart Help Desk at 646-227-2593. They are available Monday through Friday between and (Eastern time).
Managing Your Pain at Home
People have pain or discomfort for different lengths of time. You may still have some pain when you go home and will probably be taking pain medication. Some people have soreness, tightness, or muscle aches around their incision for 6 months or longer. This does not mean something is wrong.
Follow these guidelines to help manage your pain at home.
- Take your medicines as directed and as needed.
- Call your healthcare provider if the medicine prescribed for you does not help your pain.
- Do not drive or drink alcohol while you’re taking prescription pain medicine. Some prescription pain medicines can make you drowsy (very sleepy). Alcohol can make the drowsiness worse.
-
You’ll have less pain and need less pain medicine as your incision heals. An over-the-counter pain reliever will help with aches and discomfort. Acetaminophen (Tylenol®) and ibuprofen (Advil or Motrin) are examples of over-the-counter pain relievers.
- Follow your healthcare provider’s instructions for stopping your prescription pain medicine.
- Do not take too much of any medicine. Follow the instructions on the label or from your healthcare provider.
- Read the labels on all the medicines you’re taking. This is very important if you’re taking acetaminophen. Acetaminophen is an ingredient in many over-the-counter and prescription medicines. Taking too much can harm your liver. Do not take more than one medicine that has acetaminophen without talking with a member of your care team.
- Pain medicine should help you get back to your usual activities. Take enough to do your activities and exercises comfortably. You may have a little more pain as you start to be more active.
- Keep track of when you take your pain medicine. It works best 30 to 45 minutes after you take it. Taking it when you first have pain is better than waiting for the pain to get worse.
Some prescription pain medications (such as opioids) may cause constipation (having fewer bowel movements than usual).
Preventing and managing constipation
Talk with your healthcare provider about how to prevent and manage constipation. You can also follow these guidelines.
- Go to the bathroom at the same time every day. Your body will get used to going at that time. But if you feel like you need to go, don’t put it off.
- Try to use the bathroom 5 to 15 minutes after meals. After breakfast is a good time to go. That’s when the reflexes in your colon are strongest.
- Exercise, if you can. Walking is a great type of exercise that can help prevent and manage constipation.
- Drink 8 to 10 (8-ounce) cups (2 liters) of liquids daily, if you can. Choose water, juices (such as prune juice), soups, and milkshakes. Limit liquids with caffeine, such as coffee and soda. Caffeine can pull fluid out of your body.
- Slowly increase the fiber in your diet to 25 to 35 grams per day. Unpeeled fruits and vegetables, whole grains, and cereals contain fiber. If you have an ostomy or recently had bowel surgery, ask your healthcare provider before changing your diet.
-
Both over-the-counter and prescription medicines can treat constipation. Ask your healthcare provider before taking any medicine for constipation. This is very important if you have an ostomy or have had bowel surgery. Follow the instructions on the label or from your healthcare provider. Examples of over-the-counter medicines for constipation are:
- Docusate sodium (Colace®). This is a stool softener (medicine that makes your bowel movements softer) that causes few side effects. You can use it to help prevent constipation. Do not take it with mineral oil.
- Polyethylene glycol (MiraLAX®). This is a laxative (medicine that causes bowel movements) that causes few side effects. Take it with 8 ounces (1 cup) of a liquid. Only take it if you’re already constipated.
- Senna (Senokot®). This is a stimulant laxative, which can cause cramping. It’s best to take it at bedtime. Only take it if you’re already constipated.
Caring for Your Incisions After Thoracic Surgery
You will have more than 1 incision after your thoracic surgery. The location of your incisions will depend on the type of surgery you had. There will be incisions from the surgical site and the chest tube. It’s normal for the skin below your incision to feel numb. This happens because some of your nerves were cut during your surgery. The numbness will go away over time.
Surgical Incision(s)
- By the time you’re ready to leave the hospital, your surgical incision(s) will have started to heal.
- Look at your incision(s) with your nurse before you leave the hospital so you know what it looks like. This will help you know if there are any changes later.
- If any fluid is draining from your incision(s), write down the amount, color, and if it has a smell.
- If you go home with staples in your incision, your healthcare provider will take them out during your first appointment after surgery. It’s OK to get them wet.
- If you have Steri-Strips or Dermabond on your incision, they’ll loosen and fall or peel off on their own. If they have not fallen off after 10 days, you can take them off.
Chest Tube Incision
- You may have some thin, yellow or pink-colored drainage from your chest tube incision. This is normal.
- Keep your incision covered with a bandage for 48 hours (2 days) after your chest tube is removed. If it gets wet, change it as soon as possible.
- After 48 hours, if you do not have any drainage, you can remove the bandage and keep your incision uncovered.
- If you have drainage, keep wearing a bandage until the drainage stops. Change it at least once a day or more often if the bandage becomes wet.
- Sometimes, the drainage may start again after it has stopped. This is normal. If this happens, cover the area with a bandage. Call your healthcare provider if you have questions.
- You may have some soreness in your back or chest after your chest tube is removed. This will go away in a few weeks.
Sending Pictures to Your Healthcare Provider
If you’re worried about how your incision is healing, talk with your healthcare provider. You can also send a picture of your incision to your nurse. If you have an MSK My Chart account, send a picture in a message from your account. Messages are only checked on business days (Monday through Friday).
For more information about taking a good picture of your skin, read the resource Tips for Taking Pictures to Share with Your Healthcare Provider.
Showering After Thoracic Surgery
You can shower 48 hours (2 days) after your chest tube is removed. Take a shower every day to clean your incision. If you have staples in your incision, it’s OK to get them wet.
Take your bandage(s) off before you shower. Use soap during your shower, but do not put it directly on your incision. Do not rub the area around your incision.
After you shower, pat the area dry with a clean towel. Cover your incision with a bandage if your clothing may rub it or if you have drainage.
Do not take tub baths until talking with your surgeon.
Eating and Drinking After Thoracic Surgery
You can eat all the foods you did before your thoracic surgery, unless your healthcare provider gives you other instructions. Eating a balanced diet with lots of calories and protein will help you heal after surgery. Try to eat a good protein source (such as meat, fish, or eggs) at each meal. You should also try to eat fruits, vegetables, and whole grains.
It’s also important to drink plenty of liquids. Choose liquids without alcohol or caffeine. Try to drink 8 to 10 (8-ounce) glasses of liquids every day.
For more information, read Eating Well During Your Cancer Treatment. If you have questions about your diet, ask to see a clinical dietitian nutritionist.
Exercising Your Lungs After Thoracic Surgery
It’s important to exercise your lungs so they expand fully. This helps prevent pneumonia.
- Use your incentive spirometer 10 times every hour you’re awake. For more information, read How To Use Your Incentive Spirometer.
- Do coughing and deep breathing exercises. A member of your care team will teach you how.
Managing Fatigue After Thoracic Surgery
It’s common to have less energy than usual after your surgery. Recovery time is different for everyone. Increase your activities each day as much as you can. Always balance activity periods with rest periods. Rest is an important part of your recovery.
It may take some time until your normal sleep pattern returns. Try not to nap during the day. Taking a shower before bed and taking your prescribed pain medications can also help.
Your body is an excellent guide for telling you when you have done too much. When you increase your activity, monitor your body’s reaction. You may find that you have more energy in the morning or the afternoon. Plan your activities for times of the day when you have more energy.
Physical Activity and Exercise After Thoracic Surgery
When you leave the hospital, your incision may look healed on the outside, but it will not be healed on the inside. For the first 3 weeks after your surgery:
- Do not lift anything heavier than 10 pounds (4.5 kilograms).
- Do not do any high-energy activities (such as jogging and tennis).
- Do not play any contact sports (such as football).
Doing aerobic exercise, such as walking and stair climbing, will help you gain strength and feel better. Walk at least 2 to 3 times a day for 20 to 30 minutes. You can walk outside or indoors at your local mall or shopping center.
It’s normal to have less energy than usual after your surgery. Recovery time is different for each person. Increase your activities each day as much as you can. Always balance activity periods with rest periods. Rest is an important part of your recovery.
Strengthening Your Arm and Shoulder After Thoracic Surgery
Stretching exercises will help you regain full arm and shoulder movement. They will also help relieve pain on the side of your surgery.
Do the exercises in the “How to Do Stretching Exercises After Thoracic Surgery” section. Start doing them as soon as your chest tube is removed.
Use the arm and shoulder on the side of your surgery in all your activities. For example, use them when you bathe, brush your hair, and reach up to a cabinet shelf. This will help restore full use of your arm and shoulder.
Loosening Your Mucus After Thoracic Surgery
Drink liquids to help keep your mucus thin and easy to cough up. Ask your healthcare provider how much you should drink each day. For most people, this will be at least 8 to 10 (8-ounce) glasses of liquid each day.
Use a humidifier while you sleep during the winter months. Make sure to change the water and clean the humidifier often. Follow the manufacturer’s instructions.
Smoking After Thoracic Surgery
Do not smoke. Smoking is harmful to your health at any time, but it’s even more harmful as you’re healing. Smoking causes the blood vessels in your body to become narrow. This decreases the amount of oxygen that reaches your wounds as they’re healing.
Smoking can also cause problems with breathing and regular activities. It is also important to avoid places that are smoky. Your nurse can give you information to help you deal with other smokers or situations where smoke is present.
MSK has specialists who can help you quit smoking. For more information about our Tobacco Treatment Program, or to make an appointment, call 212-610-0507.
Driving After Thoracic Surgery
Ask your healthcare provider when you can drive. Do not drive while you’re taking pain medication that may make you drowsy.
You can ride in a car as a passenger at any time after you leave the hospital.
Traveling By Plane After Thoracic Surgery
Do not travel by plane until your doctor says it’s OK. They’ll talk with you about this during your first appointment after your surgery.
Sexual Activity After Surgery
Your healthcare provider will tell you when you can start having sexual activity. This is usually as soon as your incisions heal.
Going back to work
Talk with your healthcare provider about your job. They’ll tell you when it may be safe for you to start working again based on what you do. If you move around a lot or lift heavy objects, you may need to stay out a little longer. If you sit at a desk, you may be able to go back sooner.
Managing your feelings
You may have new and upsetting feelings after a surgery for a serious illness. Many people say they felt weepy, sad, worried, nervous, irritable, or angry at one time or another. You may find that you cannot control some of these feelings. If this happens, it’s a good idea to seek emotional support. Your healthcare provider can refer you to MSK’s Counseling Center. You can also reach them by calling 646-888-0200.
The first step in coping is to talk about how you feel. Family and friends can help. We can also reassure, support, and guide you. It’s always a good idea to let us know how you, your family, and your friends are feeling emotionally. Many resources are available to you and your family. We’re here to help you and your family and friends handle the emotional aspects of your illness. We can help no matter if you’re in the hospital or at home.
Follow-up Appointments
Your first appointment after surgery will be 1 to 3 weeks after you leave the hospital. Your nurse will give you instructions on how to make this appointment, including the phone number to call.
During this appointment, your surgeon will discuss the pathology results with you in detail. You may also have appointments with other healthcare providers after your surgery.
When to Call Your Healthcare Provider
Call your healthcare provider if:
- You have a fever of 101 °F (38.3 °C) or higher.
- You have swelling in your chest, neck, or face.
- You have a sudden change in your voice.
- You have not had a bowel movement for 3 days or longer.
- You have pain that does not get better with your medications.
- You’re having trouble breathing.
- The skin around your incision is warmer than usual.
- The skin around your incision is very red or getting more red.
- The area around your incision is starting to swell or getting more swollen.
- You have drainage from your incision that smells bad or is thick or yellow.
- You have any questions or concerns.
Monday through Friday from to call your healthcare provider’s office. After , during the weekend, and on holidays, call 212-639-2000. Ask to speak to the person on call for your healthcare provider.
How to Do Stretching Exercises After Thoracic Surgery
Stretching exercises will help you regain full arm and shoulder movement. You can start doing them once your chest tube is removed.
To do the exercises, follow the instructions below. One of your healthcare providers will tell you how many times to repeat each exercise.
You’ll need a straight-backed chair and a hand towel to do these exercises.
Axillary Stretch
- Sit in a straight-backed chair with your feet flat on the floor.
-
Clasp your hands together in front of you (see Figure 2).
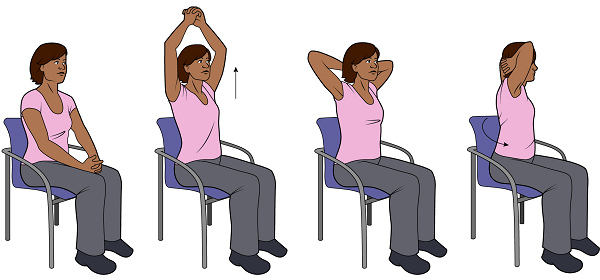
Figure 2. Axillary stretch - Keeping your hands clasped, lift your arms up and over your head.
- Slide your hands down to the back of your neck.
- Slowly twist the upper part of your body to the right. Hold this position for 5 seconds while bringing your elbows as far back as possible.
- Return to the starting position.
- Slowly twist the upper part of your body to the left. Hold this position for 5 seconds while bringing your elbows as far back as possible.
- Return to the starting position.
Towel stretch
- Stand comfortably with your feet about 6 inches (15 centimeters) apart.
-
Hold the hand towel in front of you. Hold one end in each hand (see Figure 3).
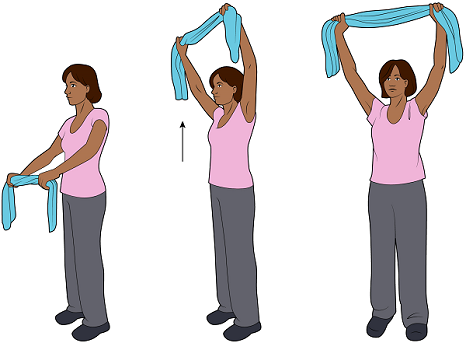
Figure 3. Stretching up - Bring your arms over your head, straighten your elbows, and stretch toward your upper back. Do not arch your back. Do not force the movement if it is difficult. Try to hold the position for 5 seconds.
- Relax and return to the starting position.
- Stand as in Step 1.
-
Grasp the towel behind your back and lift upward as far as possible (see Figure 4). Be sure to stand straight. Try to hold the position for 5 seconds.

Figure 4. Stretching back - Return to the starting position.
Additional Resources
- How To Use Your Incentive Spirometer
- Call! Don't Fall!
- What You Can Do to Avoid Falling
- Eating Well During Your Cancer Treatment
- Managing Constipation
- Communicating With Your Care Team: When to Call or Use MSK MyChart
- Common Questions About MSK's Recovery Tracker
- Frequently Asked Questions About the Goals to Discharge Checklist
