This information describes dietary (eating and drinking) guidelines to follow while your colon is healing. It also explains how to manage common side effects of having an ileostomy.
General Eating and Drinking Guidelines
Follow these guidelines for the first few weeks after your surgery. This will help keep you comfortable while your colon heals.
- Eat small meals often. Try to have 6 small meals throughout the day instead of 3 large ones. Don’t eat too much in the evening. This will help limit the bowel movements (poop) from your ileostomy during the night.
- Eat slowly and chew your food well.
- Drink 8 to 10 (8-ounce) glasses (about 2 liters) of liquids every day. This will help you replace the water lost through your ileostomy and keep you from becoming dehydrated (losing more fluid from your body than usual). For more information, read the “Preventing Dehydration” section.
- Eat mostly bland, low-fiber foods. For more information, read the “Recommended foods” section.
- When you add foods back into your diet, introduce them 1 at a time. For more information, read the “Adding foods to your diet” section.
Before you’re discharged (released) from the hospital, a clinical dietitian nutritionist will talk with you about these guidelines. After you leave the hospital, your doctor and an outpatient clinical dietitian nutritionist will help you as you go back to following your usual diet.
Recommended foods
It’s best to eat mostly bland, low-fiber foods for the first few weeks after your surgery. Bland foods are cooked, easy-to-digest foods that aren’t spicy, heavy, or fried. Eating bland foods will help you avoid uncomfortable symptoms, such as:
- Diarrhea (loose or watery bowel movements)
- Bloating
- Gas
- Swelling or tenderness at your ileostomy site
The following tables include examples of bland, low-fiber foods. If you have questions about foods not listed in these tables, call 212-639-7312 to talk with an outpatient clinical dietitian nutritionist. You can reach a staff member Monday through Friday, from to
Milk and dairy |
|
|---|---|
|
Foods to include in your diet
|
Foods to limit
|
* If you have diarrhea after having these products, try non-dairy milks, lactose-free cheese, or lactose-free yogurt instead.
** When trying eggs, start with a small amount (such as 1 egg). Eggs may cause a bad odor (smell) when you open your pouch.
Meats and proteins |
|
|---|---|
|
Foods to include in your diet
|
Foods to limit
|
* When trying fish and nut butters, start with small amounts. These foods may cause a bad odor when you open your pouch.
Grains |
|
|---|---|
|
Foods to include in your diet Low-fiber foods, such as:
|
Foods to limit High-fiber foods, such as whole grains (whole wheat bread, brown rice, bran cereal, quinoa, and buckwheat) |
Vegetables |
|
|---|---|
|
Foods to include in your diet Low-fiber foods, such as:
|
Foods to limit
Foods to avoid
|
Some vegetables may cause gas or a bad odor for some people. If a certain vegetable causes you to have gas or a bad odor, don’t eat it. For more information, read the “Guidelines for Managing Common Problems” section.
Fruits |
|
|---|---|
|
Foods to include in your diet Low-fiber foods, such as:
|
Foods to limit High-fiber foods, such as:
Foods to avoid For the first 3 to 4 weeks after your surgery, don’t eat raw fruits with the skin. Examples are:
These fruits may cause an ileostomy blockage. |
* For the first 3 to 4 weeks after your surgery, don’t eat more than 1 small ripe banana per day. Eating too much banana may cause an ileostomy blockage. For more information, read the “Preventing Ileostomy Blockage” section.
Fats |
|
|---|---|
|
Foods to include in your diet
|
Foods to limit
|
When eating fats, start with a small amount. Fats may cause discomfort.
Drinks |
|
|---|---|
|
Drinks to include in your diet
|
Drinks to limit
|
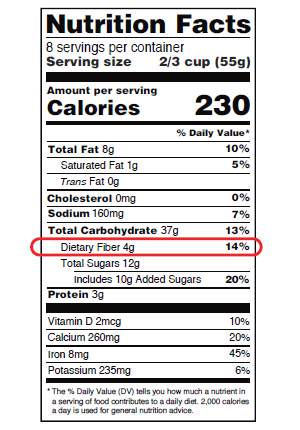
Reading Nutrition Facts labels
You can find the amount of fiber in your food by looking at the Nutrition Facts label (see Figure 1). Nutrition Facts labels can help you compare the nutritional information between different foods.
Adding foods to your diet
After your surgery, you may have some food intolerances that you didn’t have before surgery. A food intolerance is when eating a certain type of food causes uncomfortable symptoms, such as diarrhea, bloating, gas, or bad odor. Sometimes, food intolerances go away as your colon heals.
When you add foods back into your diet, introduce them 1 at a time. If a certain food causes uncomfortable symptoms, don’t eat it for a few weeks. Then try it again. No 2 people will react the same way to food. You’ll learn through experience which foods, if any, you shouldn’t eat.
For more information, read the “Guidelines for Managing Common Problems” section.
High-fiber foods
Your first follow-up appointment will be about 2 weeks after your surgery. At this appointment, your doctor will tell you if you can start adding high-fiber foods back into your diet. Doing this will help make your bowel movements bulkier (more solid).
When you start adding high-fiber foods back into your diet, do it slowly. Only add 1 food at a time. Make sure you’re also drinking enough liquids. Aim to drink 8 to 10 (8-ounce) glasses (about 2 liters) of liquids every day.
Preventing Dehydration
When you have an ileostomy, you lose much more salt, potassium, and water than usual. This can lead to dehydration.
Throughout each day, keep track of your liquid intake (how much liquid you drink). You should also keep track of your ostomy output (how much liquid comes out of your ileostomy). Record your liquid intake and ostomy output. You can use the table in the resource Liquid Intake and Ostomy Output Log. Your nurse will give you a measuring cup before you leave the hospital.
Call your doctor’s office if your output is more than 1000 milliliters (about 34 ounces) per day or is watery. They may recommend a fiber supplement or medication.
Signs of dehydration
Being dehydrated, even for less than 24 hours, can lead to kidney failure. Kidney failure happens when your kidneys can’t do their normal functions.
If you have any of the following signs of dehydration, call your doctor’s office right away. If it’s before or after , a weekend, or a holiday, call 212-639-2000. Ask to talk to the person on call (covering) for your doctor.
- Dizziness
- Dark, amber-colored urine (pee)
- Headaches
- Muscle cramps
- Dry mouth or cracked lips
- Urinating (peeing) less than usual
- Feeling more thirsty than usual
- Heart palpitations (an unusually fast, strong, or irregular heartbeat)
- Loss of appetite (not feeling hungry)
- Emptying your pouch more than usual (such as every hour)
Guidelines for preventing dehydration
Follow these guidelines to help keep you from becoming dehydrated.
-
Aim to drink 8 to 10 (8-ounce) glasses (about 2 liters) of liquids every day.
- Don’t drink more than 4 ounces (½ cup) of liquids with meals. Don’t drink any liquids for 1 hour before and 1 hour after meals. This helps make your bowel movements bulkier.
- It’s important to keep drinking lots of liquids, even if your bowel movements are watery. Drinking less liquid won’t help your bowel movements be less watery, and it can lead to dehydration.
-
Drink sports drinks (such as Gatorade or Powerade) and oral rehydration solutions (such as Pedialyte). These drinks will help replace your fluid loss quickly, especially if your ostomy output is high. A high output is more than 1000 milliliters (about 34 ounces) per day. If you don’t have these drinks, you can make your own using these ingredients:
- 4 cups (32 ounces, which is about 1 liter) of water
- 1 cup (8 ounces) of orange juice
- 8 teaspoons (40 milliliters) of sugar
- 1 teaspoon (4 milliliters) of salt
-
Limit or avoid the following foods and drinks. They can cause diarrhea or watery bowel movements, which makes you more likely to become dehydrated.
- Limit liquids with caffeine (such as caffeinated tea and coffee) and liquids high in fat (such as regular milk) to 1 cup (8 ounces) per day.
- If you drink coffee, choose a dark roast instead of a light roast. Dark roast coffee usually has less caffeine than light roast coffee because some caffeine is lost during the roasting process.
- Limit the amount of alcohol you drink for the first 3 weeks after your surgery. Alcohol can cause you to lose more fluid. Talk with your healthcare provider for more information.
- Don’t drink sugary drinks, such as juice and soda. If you want to drink juice, choose 100% fruit juice and dilute it (mix it with water) to reduce the sugar. To do this, add 1 part water to 1 part of juice (for example, 4 ounces of water mixed with 4 ounces of juice).
- Don’t have artificial sweeteners, such as sorbitol, mannitol, and xylitol. Artificial sweeteners are often found in sugar-free drinks, candies, gum, and cough drops.
- Limit liquids with caffeine (such as caffeinated tea and coffee) and liquids high in fat (such as regular milk) to 1 cup (8 ounces) per day.
-
Eat foods that contain electrolytes. Electrolytes, such as sodium and potassium, can help prevent dehydration. The following table includes examples of foods that are high in sodium and potassium.
Foods high in sodium Foods high in potassium
- Broth
- Buttermilk
- Cheese
- Commercially prepared or processed packaged foods (such as TV dinners)
- Puréed canned soups (smooth and easy to swallow)
- Salted pretzels
- Saltine crackers
- Soy sauce
- Table salt
- Tomato juice
- Bananas
- Don’t eat more than 1 small ripe banana per day for the first 3 to 4 weeks after your surgery. Eating more than this may cause an ileostomy blockage.
- Broccoli
- Coconut water
- Chicken, fish, and veal
- Orange juice without pulp
- Oranges without seeds or membrane (the thin clear or white part around each section)
- Potatoes without the skin
- Soy milk
- Tomato or vegetable soup
- Turkey
- Yogurt
Preventing Ileostomy Blockage
An ileostomy blockage (also called a bowel obstruction) is when your intestine is partly or fully blocked. It can be caused by food, scar tissue, or a twist in your intestine. If you have an ileostomy blockage, food, liquids, and gas can’t move through your intestine as they usually do.
If there’s no gas or bowel movements coming from your stoma for 6 hours and you have cramps, pain, nausea (feeling like you’re going to throw up), or all 3, call your doctor’s office right away. These symptoms are signs of an ileostomy blockage.
Guidelines for preventing an ileostomy blockage
Follow these guidelines to help keep your ileostomy from becoming blocked.
-
If you have cramps, pain, or nausea, follow these tips. They can help move food and gas through your intestine. Remember to call your doctor’s office if you haven’t passed gas or had a bowel movement in 6 hours.
- Take a warm bath to relax your abdominal (belly) muscles.
- Change your position, such as drawing your knees up to your chest while you’re lying down.
- Don’t take a laxative (medication to help you have a bowel movement). This can make the problem worse. Talk with your doctor before taking any medications.
-
Don’t eat the following foods. They can cause an ileostomy blockage.
Foods that can cause an ileostomy blockage
- Apples with the skin
- Bean sprouts
- Cabbage (raw)
- Celery
- Chinese vegetables
- Corn
- Cucumbers
- Dried fruits
- Grapes
- Green peppers
- Mushrooms
- Nuts and seeds
- Peas
- Popcorn
- Relishes and olives
- Salad greens
- Spinach
- Vegetable and fruit skins
- Whole grains
Guidelines for Managing Common Problems
This section has guidelines for changing your diet to help manage common problems. You don’t need to follow these guidelines unless you’re having the problems listed.
If certain foods caused discomfort before your surgery, they’ll still cause discomfort after your surgery.
Diarrhea
Diarrhea is having loose or watery bowel movements, having more bowel movements than what’s normal for you, or both. Diarrhea can be caused by:
- Certain foods
- Skipping meals
- Food poisoning
- An infection in your intestine
- Antibiotics (medicines to treat infections) and other prescription medications
- A blockage in your intestine
If you’re having diarrhea, follow these guidelines:
- Call your doctor’s office. They may give you a medication to help.
- Drink 8 to 10 (8-ounce) glasses (about 2 liters) of liquids throughout the day. Drink sports drinks (such as Gatorade or Powerade) and oral rehydration solutions (such as Pedialyte), if you can.
-
Don’t eat the following foods and drinks. They may cause diarrhea.
Foods that may cause diarrhea
- Alcohol (such as beer and wine)
- Bran
- Broccoli
- Brussels sprouts
- Cabbage
- Caffeinated drinks, especially hot drinks
- Chocolate
- Corn
- Foods with artificial sweeteners (such as mannitol, sorbitol, and xylitol)
- Fried meats, fish, and poultry
- Fruit juice (such as prune, apple, grape, and orange juices)
- Green leafy vegetables
- High-fat foods
- High-sugar foods
- Legumes (such as cooked or dried beans)
- Licorice
- Milk and dairy products with lactose, if you’re lactose intolerant
- Nuts and seeds
- Peas
- Spicy foods
- Stone fruits (such as apricots, peaches, plums, and prunes)
- “Sugar-free” canned or dried fruits
- Tomatoes
- Turnip greens
- Whole grains (such as wheat bread)
- Eat more of the following foods. They may help thicken your bowel movements.
| Foods that may help thicken bowel movements | |
|---|---|
|
|
* These foods are whole grains. You can eat them if you’re having diarrhea because they may help thicken your bowel movements.
Constipation
Constipation is having fewer than 3 bowel movements per week, having hard bowel movements, having a hard time passing bowel movements, or all 3. Constipation can be caused by:
- Certain pain medications
- Certain anti-nausea medications
- Not eating enough fiber
- Not exercising enough
- Not drinking enough liquids
If you’re constipated, follow these guidelines:
- Call your doctor’s office. They may give you a medication to help.
- Drink hot water with lemon or lemon juice, coffee, or prune juice.
- Do light exercise (such as walking), if you can.
- Ask your doctor if eating high-fiber foods or taking a fiber supplement will help.
Gas and odor
For the first few weeks after your surgery, it’s common to have gas in your pouch and a bad odor when you open your pouch. You may have more gas if you had a robotic surgery.
If you’re having problems with gas or odor, talk with your wound, ostomy, and continence (WOC) nurse. You can also follow these guidelines:
-
Don’t do these things. They can cause gas.
- Chewing gum
- Drinking with a straw
- Smoking or chewing tobacco
- Eating too fast
- Skipping meals
- Ask your healthcare provider if you can take an over-the-counter medication (such as Beano® or simethicone) before meals to help prevent gas.
-
Eat less of the following foods. They may cause gas, bad odor, or both.
Foods that may cause gas, bad odor, or both
- Asparagus
- Alcohol, especially beer
- Broccoli
- Brussels sprouts
- Cabbage
- Carbonated drinks (such as soda)
- Cauliflower
- Corn
- Dried beans and peas
- Eggs
- Fish
- Garlic
- Grapes
- Leeks
- Milk and dairy products with lactose, if you’re lactose intolerant
- Onions
- Peanuts
- Prunes
-
Eat more of the following foods. They may help prevent gas, bad odor, or both.
Foods that may prevent gas, bad odor, or both
- Buttermilk
- Cranberry juice
- Kefir
- Parsley
- Yogurt
When to Call Your Healthcare Provider
Call your healthcare provider if you have any of the following:
- Any signs of dehydration
- No gas or bowel movements coming from your stoma for 6 hours and you have cramps, pain, nausea, or all 3
- Diarrhea and a fever of 100.4 °F (38 °C) or higher
- Diarrhea and you’re vomiting (throwing up)
- Diarrhea that doesn’t stop after 24 hours
- Diarrhea and smelly discharge (fluid), or forceful liquid output from your stoma
If you have questions about your diet, call 212-639-7312 to talk with an outpatient clinical dietitian nutritionist. You can reach a staff member Monday through Friday, from to
