This information will help you get ready for your LDR brachytherapy (BRAY-kee-THAYR-uh-pee) treatment to your prostate at MSK.
Read through this resource at least once before your brachytherapy. Use it as a reference in the days leading up to your treatments.
About your prostate
Your prostate is a small, firm gland about the size of a walnut. It works with other glands in your body to make semen.
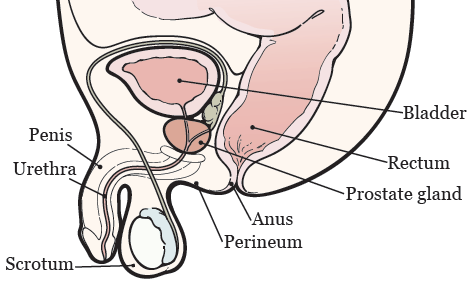
Your prostate is in front of your rectum, below your bladder (see Figure 1). It surrounds your urethra, the tube that drains urine (pee) from your bladder.
About brachytherapy
Brachytherapy is a type of radiation therapy used to treat prostate cancer.
Radiation therapy uses high-energy radiation to treat cancer. It works by damaging the cancer cells and making it hard for them to multiply. Your body can then naturally get rid of the damaged cancer cells. Radiation therapy also affects normal cells, but they can repair themselves in a way that cancer cells can’t.
With brachytherapy, your healthcare provider will place tiny radioactive implants (also called seeds) inside your prostate. Each one is about the size of a sesame seed. The seeds will give off radiation for a period of time and then stop. They’ll stay in your prostate for the rest of your life.
About the radioactive seeds
The radioactive seeds will be made of radioactive iodine (I-125) or palladium (Pd-103) and covered with titanium. Your radiation oncologist will tell you which is the best choice for you. Your healthcare provider will place 50 to 125 seeds in your prostate. How many they place depends on how big your prostate is.
A radiation safety officer will give you a card to keep with you after your procedure. The card says you’re getting radiation therapy and has the date when the radiation will be done. If you need to go to a hospital for any reason before the date on the card, tell the healthcare provider you’ve had radioactive seeds implanted.
Your role on your radiation therapy team
You’ll have a team of healthcare provider working together to care for you. You’re a part of that team, and your role includes:
- Getting to your appointments on time.
- Asking questions and talking about your concerns.
- Telling us when you have side effects.
- Telling us if you’re in pain.
-
Caring for yourself at home by:
- Quitting smoking if you smoke. MSK has specialists who can help. To learn more about our Tobacco Treatment Program, call 212-610-0507. You can also ask your nurse about the program.
- Drinking liquids based on our instructions.
- Eating or avoiding the foods and drinks we suggest.
- Staying around the same weight.
Before your LDR brachytherapy procedure
Getting ready for your procedure
You and your care team will work together to get ready for your procedure. Help us keep you safe by telling us if any of these things apply to you, even if you’re not sure.
You may need to follow special instructions before your procedure based on the medicines and supplements you take. If you do not follow those instructions, your procedure may be delayed or canceled.
-
I take any prescription medicines. A prescription medicine is one you can only get with a prescription from a healthcare provider. Examples include:
- Medicines you swallow.
- Medicines you take as an injection (shot).
- Medicines you inhale (breathe in).
- Medicines you put on your skin as a patch or cream.
- I take any over-the-counter medicines, including patches and creams. An over-the-counter medicine is one you can buy without a prescription.
- I take any dietary supplements, such as herbs, vitamins, minerals, or natural or home remedies.
- I have a pacemaker, automatic implantable cardioverter-defibrillator (AICD), or other heart device.
- I have had a problem with anesthesia (A-nes-THEE-zhuh) in the past. Anesthesia is medicine to make you sleep during a surgery or procedure.
- I’m allergic to certain medicines or materials, including latex.
- I’m not willing to receive a blood transfusion.
- I use recreational drugs, such as marijuana.
About drinking alcohol
It’s important to talk with your healthcare providers about how much alcohol you drink. This will help us plan your care.
If you drink alcohol regularly, you may be at risk for problems during and after your procedure. These include bleeding, infections, heart problems, and a longer hospital stay.
If you drink alcohol regularly and stop suddenly, it can cause seizures, delirium, and death. If we know you’re at risk for these problems, we can prescribe medications to help prevent them.
Here are things you can do before your procedure to keep from having problems.
- Be honest with your healthcare providers about how much alcohol you drink.
-
Try to stop drinking alcohol once your procedure is planned. Tell your healthcare provider right away if you:
- Get a headache.
- Feel nauseous (like you’re going to throw up).
- Feel more anxious (nervous or worried) than usual.
- Cannot sleep.
- Tell your healthcare provider if you cannot stop drinking.
- Ask your healthcare provider questions about drinking and procedures. All your medical information will be kept private, as always.
About smoking
If you smoke or use an electronic smoking device, you can have breathing problems when you have a procedure. Vapes and e-cigarettes are examples of electronic smoking devices. Stopping for even a few days before your procedure can help prevent breathing problems during and after your procedure.
Your healthcare provider will refer you to our Tobacco Treatment Program if you smoke. You can also reach the program by calling 212-610-0507.
About sleep apnea
Sleep apnea is a common breathing problem. If you have sleep apnea, you stop breathing for short lengths of time while you’re asleep. The most common type is obstructive sleep apnea (OSA). With OSA, your airway becomes fully blocked during sleep.
OSA can cause serious problems during and after a procedure. Tell us if you have or think you might have sleep apnea. If you use a breathing device, such as a CPAP machine, bring it on the day of your procedure.
Within 30 days of your procedure
Presurgical testing (PST)
You’ll have a PST appointment before your procedure. You’ll get a reminder from your healthcare provider’s office with the appointment date, time, and location. Visit www.msk.org/parking for parking information and directions to all MSK locations.
You can eat and take your usual medicines the day of your PST appointment.
It’s helpful to bring these things to your appointment:
- A list of all the medicines you’re taking, including prescription and over-the-counter medicines, patches, and creams.
- Results of any medical tests done outside of MSK in the past year, if you have them. Examples include results from a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
You’ll meet with an advance practice provider (APP) during your PST appointment. They work closely with MSK’s anesthesiology (A-nes-THEE-zee-AH-loh-jee) staff. These are doctors with special training in using anesthesia during a procedure.
Your APP will review your medical and surgical history with you. You may have tests to plan your care, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your APP may recommend you see other healthcare providers. They’ll also talk with you about which medicine(s) to take the morning of your procedure.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Fill out a Health Care Proxy form
If you have not already filled out a Health Care Proxy form, we recommend you do now. If you already filled one out or have any other advance directives, bring them to your next appointment.
A health care proxy is a legal document. It says who will speak for you if you cannot communicate for yourself. This person is called your health care agent.
- To learn about health care proxies and other advance directives, read Advance Care Planning for People With Cancer and Their Loved Ones.
- To learn about being a health care agent, read How to Be a Health Care Agent.
Talk with a member of your care team if you have questions about filling out a Health Care Proxy form.
Do physical activity
Doing physical activity will help your body get into its best condition for your procedure. It will also make your recovery faster and easier.
Try to do physical activity every day. Any activity that makes your heart beat faster, such as walking, swimming, or biking, is a good choice. If it’s cold outside, use stairs in your home or go to a mall or shopping center
Follow a healthy diet
Follow a well-balanced, healthy diet before your procedure. If you need help with your diet, talk with your healthcare provider about meeting with a clinical dietitian nutritionist.
Buy your supplies
You’ll need to buy the following supplies:
- Bisacodyl (Dulcolax®) 5 milligram (mg) tablets. You can buy them at your local pharmacy without a prescription. They’re usually sold as a box of 10 tablets, but you’ll only need to take 1 tablet.
- NuLYTELY® solution and flavor packs (cherry, lemon-lime, orange, and pineapple). Your healthcare provider will give you a prescription for this. It comes in a 1-gallon (128-ounce) bottle, but you’ll only need to drink ½ gallon (64 ounces).
- Clear liquids to drink while you’re following a clear liquid diet. Examples are listed in the “Clear Liquid Diet” table.
7 days before your procedure
Follow your healthcare provider’s instructions for taking aspirin
Aspirin can cause bleeding. If you take aspirin or a medicine that has aspirin, you may need to change your dose or stop taking it 7 days before your procedure. Follow your healthcare provider’s instructions. Do not stop taking aspirin unless they tell you to.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
Stop taking vitamin E, multivitamins, herbal remedies, and other dietary supplements
Vitamin E, multivitamins, herbal remedies, and other dietary supplements can cause bleeding. Stop taking them 7 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read Herbal Remedies and Cancer Treatment.
2 days before your procedure
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
1 day before your procedure
Get the NuLYTELY mixture ready
On the morning of the day before your procedure:
- Add lukewarm water to the NuLYTELY bottle. Fill it to the top of the line on the bottle.
- Add a flavor pack if you want to. Only use a flavor pack that came with the NuLYTELY.
- Put the cap on the NuLYTELY bottle. Shake the bottle until the powder dissolves. The mixture will be clear, even if you used a flavor pack.
- Put the bottle in the refrigerator to chill it if you want to. Many people have told us that NuLYTELY tastes better cold.
Don’t mix the NuLYTELY earlier than the morning of the day before your procedure.
Follow a clear liquid diet
You can have solid food for breakfast and lunch. Finish your lunch by (noon).
After lunch on the day before your procedure, start following a clear liquid diet. A clear liquid diet includes only liquids you can see through. Examples are listed in the “Clear Liquid Diet” table. While you’re following this diet:
- Don’t eat any solid foods.
- Try to drink at least 1 (8-ounce) glass of clear liquid every hour while you’re awake.
- Drink different types of clear liquids. Don’t just drink water, coffee, and tea.
- Don’t drink more than 2 cups (16 ounces) of liquids with caffeine.
- Don’t drink diet liquids, even if you have diabetes. If you do, you may feel weak or dizzy.
| Clear liquid diet | ||
|---|---|---|
| OK to have | Do not have | |
| Soups |
|
|
| Sweets |
|
|
| Drinks |
|
|
Take a bisacodyl tablet
At on the day before your procedure, swallow 1 (5 mg) bisacodyl tablet with a glass of water.
Drink the NuLYTELY mixture
At on the day before your procedure, start drinking the NuLYTELY mixture.
- Drink 1 (8-ounce) glass of the mixture every 15 minutes.
- Only drink half of the bottle (64 ounces). You can use the markings on the bottle to help you keep track.
- Once you’ve finished half of the NuLYTELY mixture, dump out the other half. Then, keep drinking clear liquids.
The NuLYTELY will cause frequent bowel movements, so be sure to be near a bathroom when you start drinking it. To help prevent irritation, you can apply petroleum jelly (Vaseline®) or A&D® ointment to the skin around to your anus after every bowel movement.
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-7606.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
Visit www.msk.org/parking for parking information and directions to all MSK locations.
If you have any changes in your health or need to cancel your procedure for any reason, call your radiation oncologist.
Take your medicines as instructed
Take the medicines your healthcare provider told you to take the night before your procedure. Take them with a small sip of water.
Shower
Shower using soap and water the night before or the morning of your procedure.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
The day of your LDR brachytherapy procedure
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Things to remember
- Take the medicines your healthcare provider told you to take the morning of your procedure. Take them with a small sip of water.
- Don’t wear any lotion, cream, deodorant, powder, or cologne.
- Don’t wear any metal objects. Remove all jewelry, including body piercings. The tools used during your procedure can cause burns if they touch metal.
- Leave valuable items at home.
- If you wear contact lenses, wear your glasses instead. If you don’t have glasses, bring a case for your contacts.
What to bring
- A pair of loose-fitting pants, such as sweatpants.
- Brief-style underwear that’s 1 to 2 sizes larger than you normally wear.
- Sneakers that lace up. You may have some swelling in your feet. Lace-up sneakers can accommodate this swelling.
Once you’re in the hospital
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or a similar name may be having a procedure on the same day.
When it’s time to change for your procedure, you’ll get a hospital gown, robe, and nonskid socks to wear.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicine, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
Get ready for your procedure
When it’s time for your procedure, you’ll need to remove your hearing aids, dentures, prosthetic device(s), wig, and religious articles, if you have them. You’ll either walk into the operating room or a staff member will bring you there on a stretcher.
A member of the operating room team will help you onto the operating bed. They’ll also place compression boots on your lower legs. These gently inflate and deflate to help blood flow in your legs. Once you’re comfortable, your anesthesiologist will give you anesthesia through your IV line and you’ll fall asleep. You’ll also get fluids through your IV line during and after your procedure.
During your procedure
After you’re fully asleep, your care team will place a breathing tube through your mouth into your windpipe to help you breathe. They’ll also place a urinary (Foley) catheter in your bladder to drain your urine during your procedure.
After the Foley catheter is in place, your healthcare provider will use rectal ultrasound to see your prostate. They’ll put tiny needles through your perineum into your prostate. Your perineum is the area of skin between your scrotum and anus (see Figure 1). Your healthcare provider will use a computer to determine the best place to place the seeds. Then, they’ll place the seeds in your prostate through the needles.
You’ll have a computed tomography (CT) scan to make sure all the seeds are in the right place. Then, your healthcare provider will remove the needles and Foley catheter.
After your LDR brachytherapy procedure
In the hospital
You’ll wake up in the Post-Anesthesia Care Unit (PACU). A nurse will be keeping track of your body temperature, pulse, blood pressure, and oxygen levels. They’ll also make sure you can urinate (pee) on your own.
You may have some pain after your procedure. Your healthcare providers will ask you about your pain often. They’ll give you medicine to treat your pain as needed. If your pain isn’t relieved, tell one of your healthcare providers.
Your nurse will discuss your discharge instructions with you and your caregiver.
Meet with your radiation safety officer
You’ll meet with a radiation safety officer from the Radiation Safety Service. They’ll check the level of radiation in your body. They’ll also give you a wallet card to keep after your procedure that explains the radiation. It will have the date when the radiation will be done. If you need to go to a hospital for any reason before the date on the card, tell the healthcare provider you’ve had radioactive seeds implanted.
The radiation safety officer may also give you instructions about any radiation precautions you need to take around your family and friends.
At home
Straining your urine
Although it’s very rare, you may pass a seed with your urine. This won’t affect your treatment. Your nurse will give you a strainer before you’re discharged from the hospital. Use it to strain your urine for the first 4 days after your procedure. If you pass a seed during the first 4 days, keep straining your urine for 4 more days.
If you pass a seed, don’t touch it with your hands or fingers. Pick it up with a spoon or a pair of tweezers. Place it in a small covered container, such as an empty jar. Store it away from people. Call your radiation oncologist or the Radiation Safety Service at 212-639-7391 for more instructions.
Other instructions
- If you have any bleeding on your perineum, apply steady pressure with a clean, dry washcloth or gauze for 5 minutes. If the bleeding becomes heavy or doesn’t stop, call your healthcare provider.
- It’s OK to follow your usual diet. You may want avoid things that may irritate your bladder. These include caffeine (such as coffee and tea), alcohol, citrus juices, and spicy foods.
- You can shower 24 hours after you’re discharged from the hospital.
- Don’t lift anything over 20 pounds (9.1 kilograms) for 1 week after your procedure.
- Most people can go back to work 2 days after their procedure. If heavy lifting is part of your job, ask your healthcare provider when you can go back to work.
Follow-up care
You’ll have regular appointments with your healthcare provider after your LDR brachytherapy. At each of these visits, your radiation therapy team will check how your body and the cancer are responding to your treatment. You’ll have a physical exam and blood tests, including a prostate-specific antigen test (PSA). Your healthcare provider will also help you manage any symptoms you have. Use these visits to ask questions and discuss your concerns.
Side effects of LDR brachytherapy for prostate cancer
Urinary symptoms
Urinary symptoms are the most common side effects of brachytherapy. After your procedure, you may have some of the following symptoms.
- Some people can’t urinate after the procedure or may only be able to urinate a few drops at a time. This is an emergency. Call your healthcare provider right away if you can’t urinate.
- You may need to urinate more often than usual, as many as 1 or more times an hour. This usually starts 2 to 4 weeks after the seeds are placed and can last several months or longer.
- You may feel burning when you urinate. This usually starts 2 to 4 weeks after the seeds are placed and can last for about 4 months to 1 year.
- You may notice blood in your urine, which will make it look pink. This is common and usually goes away 3 to 7 days after the seeds are placed. Call your healthcare provider if your urine is still pink after 7 days or if you pass blood clots in your urine.
- You may have bruising around your scrotum and penis. This should go away 1 to 2 weeks after your procedure. Call your healthcare provider if you still have bruising after 2 weeks.
Talk with your healthcare provider if you have any of these symptoms. If you have a procedure to look at your bladder (such as a cystoscopy) planned, wait to have it until after you’ve talked with your healthcare provider.
Bowel symptoms
- Your bowel movements may happen more often or be softer than usual. This happens when your rectum is irritated. It may start 1 week after the seeds are placed and can last several months or longer.
- You may have rectal discomfort or mucus discharge.
- If you have hemorrhoids, they may get worse.
Talk with your healthcare provider if you have any bowel symptoms. If you have a procedure to look into your rectum or colon planned (such as a colonoscopy), wait to have it until after you’ve talked with your healthcare provider.
Erectile dysfunction (ED)
Erectile dysfunction, sometimes called impotence, means having trouble or not being able to get an erection. You may notice a change in the strength of your erection. You may have less semen or the consistency of your semen may be different.
Out of every 10 people who have LDR brachytherapy to their prostate, around 3 people develop ED within 5 years of their procedure and around 7 don’t. It’s difficult to predict who will develop ED.
If you develop ED, it may be permanent. Tell your healthcare provider if it happens. There are many treatments for ED available.
Radiation safety instructions
The radioactive seeds in your prostate are made of palladium (Pd-103) or Iodine (I-125). If you’re not sure which type you have, ask your healthcare provider.
If you had palladium implants, you don’t need to follow any safety precautions. If you had iodine (I-125) implants, follow these instructions.
The seeds give off a very small amount of radiation. The amount of radiation gets smaller the further it gets from your body. There’s no measurable radiation 3 feet (1 meter) away.
You can’t make something radioactive by touching it. You don’t have to do anything special with linens, clothing, dishes, or in the bathroom. The seeds won’t disturb pacemakers or microwave ovens.
Make sure to follow all the instructions on the card that your radiation safety officer gave you, including avoiding holding children on your lap and sleeping with your partner in a spoon shaped position.
Safe sex precautions
You can start having sexual activity again 1 week after your procedure.
Rarely, a seed can pass from your prostate when you ejaculate. Use a condom or ejaculate outside your partner at least the first 5 times you ejaculate after your procedure. If your partner is pregnant, use a condom until the baby is born. This lets you check for a seed. It may also lessen any worry you have about being able to ejaculate after your procedure.
Call your radiation oncologist or radiation safety officer if you lose a seed when you ejaculate. Pick up and store the seed following the instructions in the “Straining your urine” section.
Traveling
You can travel, including on airplanes. Bring the wallet card your radiation safety officer gave you. Some security equipment may detect radioactivity or metal.
Bodily fluids
The radiation from the seeds won’t get into your blood, urine, or other body fluids. You don’t need to follow any special steps.
Support services
Admitting Office
212-639-7606
Call if you have questions about your hospital admission, such as asking for a private room.
Anesthesia
212-639-6840
Call if you have questions about anesthesia.
Male Sexual and Reproductive Medicine Program
646-888-6024
Cancer and cancer treatments can affect your sexual health, fertility, or both. Our Male Sexual and Reproductive Medicine Program can help with sexual health problems, such as erectile dysfunction (ED). We can help before, during, or after your treatment. Call for more information or to make an appointment.
Patient Representative Office
212-639-7202
Call if you have questions about the Health Care Proxy form or concerns about your care.
Social Work
www.msk.org/socialwork
212-639-7020
Social workers help patients, families, and friends deal with common issues for people who have cancer. They provide individual counseling and support groups throughout your treatment. They can help you communicate with children and other family members.
Our social workers can also help refer you to community agencies and programs. They also have information about financial resources, if you’re having trouble paying your bills.
When to call your healthcare provider
Call your healthcare provider if you have:
- A fever of 101 °F (38.3 °C) or higher.
- Pain that doesn’t get better with your medicines.
- Any new symptom(s) or physical change(s).