This resource explains what urinary incontinence is and how to manage it after prostate treatment.
About your bladder
Your bladder (see Figure 1) is an organ that holds urine (pee). As urine flows into your bladder, the walls of your bladder stretch. This helps make room for more liquid.

When you urinate (pee), your bladder pushes urine out of your body through your urethra (yoo-REE-thruh). The urethra is the tube that carries urine from your bladder to outside your body. While this happens, the muscles in your urethra and pelvis relax.
About urinary incontinence
Urinary continence is being able to stop urine from accidentally leaking from your bladder. Incontinence (in-KON-tih-nents) is when urine leaks accidentally.
Incontinence can happen right after prostate treatment or later as a long-term side effect. This depends on what type of prostate treatment you had.
Incontinence may happen in people who have had radical prostatectomy (PROS-tuh-TEK-toh-mee) surgery. This often happens right after the surgery and almost fully goes away by 12 months after surgery. If incontinence does not go away after 12 months, you may need to see a urologist to further manage it. A urologist is a doctor with special training in the urinary system.
Incontinence can also happen in people who have had transurethral (TRANZ-yoo-REE-thrul) resection of the prostate after radiation therapy.
Stress incontinence
This is a loss of urine caused by pressure on the bladder from physical activity, including sneezing, coughing, or exercise.
Urge incontinence
This is a sudden and intense urge to urinate that makes you leak urine. This can happen when the muscles in your bladder squeeze down too often, too strong, or both. Read About Overactive Bladder (OAB) to learn more.
How to treat incontinence after prostate treatment
There are a few ways to treat incontinence after prostate treatment. Your healthcare provider will talk with you about which treatment is right for you.
Non-surgical treatments
When possible, your healthcare provider will recommend non-surgical incontinence treatments before treating incontinence with surgery. Here are some ways to manage incontinence without surgery.
Pelvic floor muscle (Kegel) exercises or training
Pelvic floor muscle exercises or training are recommended for people who have had a radical prostatectomy. You can start Kegel exercises as soon as your catheter is removed. Do not do Kegel exercises while your catheter is in place. Read Pelvic Floor Muscle (Kegel) Exercises for Males to learn more.
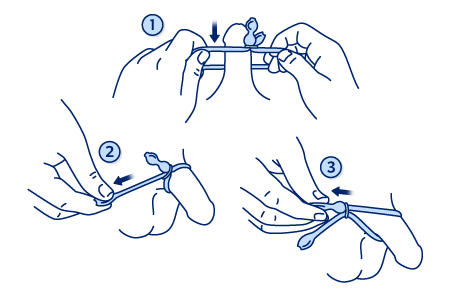
UroStop® for sexual incontinence
Sexual incontinence is when urine leaks from your penis during sex. UroStop is a small, non-surgical device that you wear on your penis during sex (see Figure 2).
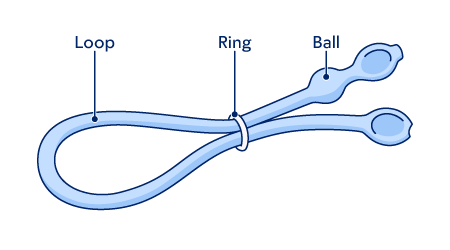
It gently squeezes the urethra to stop urine from leaking during sex (see Figure 3).
Other treatments and procedures
Your healthcare provider may recommend other treatments for incontinence after prostate treatment, such as urinary pads or incontinence clamps. An incontinence clamp puts slight pressure on the urethra to prevent urine from leaking. Read How to Use Your Incontinence Clamp to learn more.
Your healthcare provider may offer these along with another procedure, or as a few smaller procedures.
Surgical treatments
Some people have trouble with stress urinary incontinence after prostate treatment. Your healthcare provider may offer surgery if this bothers you and does not improve after 6 months of treatment. They may also recommend surgery if incontinence does not improve after 1 year of treatment.
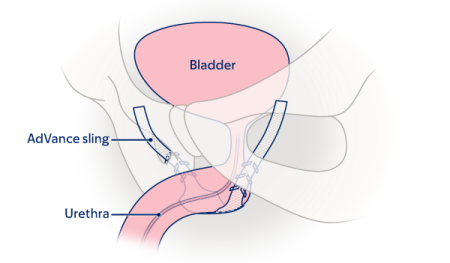
Male sling surgery
A male sling is a common surgical treatment for people with mild (not bad) to moderate stress urinary incontinence after prostate treatment. The sling is a strip of mesh that acts like a hammock (see Figure 4). It’s made to lift and support the urethra. This helps your urinary sphincter stay closed and prevent leaks. Slings are not often recommended for people with severe (very bad) stress incontinence.
Read About Your Advance™ XP Male Sling System and Placement Surgery to learn more.
Adjustable balloon devices
An adjustable balloon is an implant that works by inflating a small balloon at the end of the implant. This squeezes the lower part of the bladder closed to stop urine from leaking (see Figure 5).
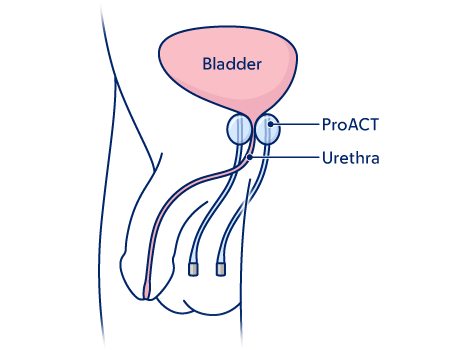
Your healthcare provider may recommend an adjustable balloon device if:
- You have not had radiation.
- You have mild to moderate stress urinary incontinence after prostate treatment.
A surgeon will place the balloon through two small incisions on either side of the perineum (below the scrotum). The balloon is usually filled with contrast and saline. Your healthcare provider can adjust how much the balloon is filled in clinic as needed.
Artificial urinary sphincter (AUS)
An AUS is a device that works like your natural urinary sphincter (see Figure 6). Your natural urinary sphincter is a muscle that controls the flow of urine out of your bladder. When your urinary sphincter is contracted (closed), it blocks the opening of your bladder. This stops urine from leaking out.
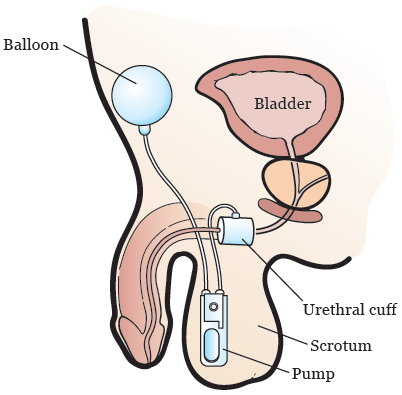
An AUS is recommended for people who:
- Have mild to severe stress urinary incontinence after prostate treatment.
- Had radiotherapy and want surgery to manage incontinence.
- Had a sling and stress urinary incontinence comes back or gets worse.
Before getting an AUS, your healthcare provider should make sure you’re able to use it properly.
If stress urinary continence continues or comes back after getting an AUS, talk with your healthcare provider.
Artificial urinary sphincters last an average of 8 years. As they wear down over time, your healthcare provider may remove it and place a new one.
If you had urethral reconstructive surgery, you may be more likely to have problems with an AUS. Talk with your healthcare provider.
Read About Your Artificial Urinary Sphincter (AUS) to learn more.
When to call your healthcare provider
Call your healthcare provider if: you have:
- You have a fever of 101° F (38.3° C) or higher.
- You have new pain at the surgical site.
- You have blood in your urine.
- You have trouble urinating (peeing).
- You feel new burning when you urinate.
- You have pus or discharge from surgical site.
- Your incontinence gets worse.
- You have other symptoms.
MSK resources
MSK Incontinence Specialist
If you think a consultation with a urologic surgeon may help you, talk with your healthcare provider. They may refer you to a functional and reconstructive urologist who has special training in treating incontinence.