This information will help you get ready for your rigid bronchoscopy (bron-KOS-koh-pee) at MSK. It also explains what to expect before, during, and after your procedure.
About your rigid bronchoscopy
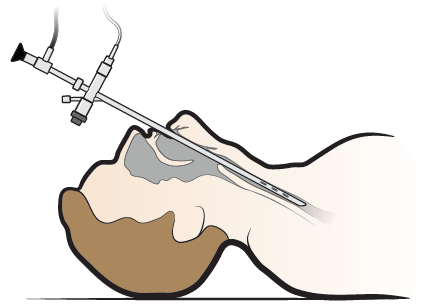
A bronchoscopy is a procedure that lets your doctor look inside your lung airways using a bronchoscope (BRON-koh-SKOPE). A bronchoscope is a thin tube with a light and camera on the end of it.
Your doctor will place the bronchoscope in your mouth. They will gently move it down your throat, through your trachea (windpipe), and into your airways.
During your rigid bronchoscopy, your doctor can:
- Control any bleeding you have.
- Reduce the size of a tumor.
- Place a stent (a hollow tube that helps keep your airway open). If you need a stent, read Tracheal or Bronchial Stent Placement.
- Remove things that should not be in your lungs, such as food or pills.
- Do a biopsy (a procedure to get tissue samples), if needed.
Make sure to tell your doctor before your procedure if you have any of the following:
- Head or neck problems, such as stiffness or dental issues.
- Surgery or radiation on your head or neck.
- Rheumatoid arthritis (ROO-muh-TOYD ar-THRY-tis). Rheumatoid arthritis is a disorder that causes swollen and painful joints.
Your healthcare provider will give you information and talk with you about what to expect during your procedure. They will also tell you where your procedure will be done. They will check off the correct box below to help you remember.
Your bronchoscopy will be done at one of these locations in Memorial Hospital, the main hospital at MSK:
-
Endoscopy suite
1275 York Ave. (between East 67th and East 68th streets)
New York, NY 10065
Take the B elevator to the 2nd floor. Turn right and enter the Surgery and Procedural Center through the glass doors. -
Operating room
1275 York Ave. (between East 67th and East 68th streets)
New York, NY 10065
Take the B elevator to the Presurgical Center (PSC) on the 6th floor.
Visit www.msk.org/parking for parking information and directions to all MSK locations.
What to do before your rigid bronchoscopy
Talk with a nurse and plan your care
Before your procedure, you’ll talk with a nurse to plan your care during your procedure. The way you talk with the nurse depends on where your procedure will be done. Your healthcare provider will tell you what to expect.
Presurgical testing (PST)
Your healthcare provider will tell you if you need presurgical testing (PST) before your procedure. PST is a regular physical exam. It can also include other medical tests that will give your care team important information about your health. PST helps your care team find out if you’re healthy enough to have the procedure.
If you need PST, you will be scheduled for an appointment within 30 days (1 month) of your procedure. The date, time, and location will be printed on the appointment reminder from your healthcare provider’s office. You can eat and take your usual medications the day of your appointment.
It’s helpful to bring these things to your PST appointment:
- A list of all the medications you’re taking, including prescription and over-the-counter medications, patches, and creams.
- Results of any tests done outside of MSK, such as a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
During your PST appointment, you’ll meet with a nurse practitioner (NP). They work closely with anesthesiology staff (specialized healthcare providers who will give you anesthesia during your procedure). Your NP will review your medical and surgical history with you. You may also have medical tests to help plan your procedure, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your NP may recommend you see other healthcare providers. They will also talk with you about which medications to take the morning of your procedure.
Getting ready for your procedure
You and your care team will work together to get ready for your procedure. Help us keep you safe by telling us if any of these things apply to you, even if you’re not sure.
You may need to follow special instructions before your procedure based on the medicines and supplements you take. If you do not follow those instructions, your procedure may be delayed or canceled.
-
I take any prescription medicines. A prescription medicine is one you can only get with a prescription from a healthcare provider. Examples include:
- Medicines you swallow.
- Medicines you take as an injection (shot).
- Medicines you inhale (breathe in).
- Medicines you put on your skin as a patch or cream.
- I take any over-the-counter medicines, including patches and creams. An over-the-counter medicine is one you can buy without a prescription.
- I take any dietary supplements, such as herbs, vitamins, minerals, or natural or home remedies.
- I have a pacemaker, automatic implantable cardioverter-defibrillator (AICD), or other heart device.
- I have had a problem with anesthesia (A-nes-THEE-zhuh) in the past. Anesthesia is medicine to make you sleep during a surgery or procedure.
- I’m allergic to certain medicines or materials, including latex.
- I’m not willing to receive a blood transfusion.
- I use recreational drugs, such as marijuana.
About drinking alcohol
It’s important to talk with your healthcare providers about how much alcohol you drink. This will help us plan your care.
If you drink alcohol regularly, you may be at risk for problems during and after your procedure. These include bleeding, infections, heart problems, and a longer hospital stay.
If you drink alcohol regularly and stop suddenly, it can cause seizures, delirium, and death. If we know you’re at risk for these problems, we can prescribe medications to help prevent them.
Here are things you can do before your procedure to keep from having problems.
- Be honest with your healthcare providers about how much alcohol you drink.
-
Try to stop drinking alcohol once your procedure is planned. Tell your healthcare provider right away if you:
- Get a headache.
- Feel nauseous (like you’re going to throw up).
- Feel more anxious (nervous or worried) than usual.
- Cannot sleep.
- Tell your healthcare provider if you cannot stop drinking.
- Ask your healthcare provider questions about drinking and procedures. All your medical information will be kept private, as always.
About smoking
If you smoke or use an electronic smoking device, you can have breathing problems when you have a procedure. Vapes and e-cigarettes are examples of electronic smoking devices. Stopping for even a few days before your procedure can help prevent breathing problems during and after your procedure.
Your healthcare provider will refer you to our Tobacco Treatment Program if you smoke. You can also reach the program by calling 212-610-0507.
About sleep apnea
Sleep apnea is a common breathing problem. If you have sleep apnea, you stop breathing for short lengths of time while you’re asleep. The most common type is obstructive sleep apnea (OSA). With OSA, your airway becomes fully blocked during sleep.
OSA can cause serious problems during and after a procedure. Tell us if you have or think you might have sleep apnea. If you use a breathing device, such as a CPAP machine, bring it on the day of your procedure.
Ask about your medicines
You may need to stop taking some of your usual medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking.
We’ve included some common examples below, but there are others. Make sure your care team knows all the prescription and over-the-counter medicines you take. A prescription medicine is one you can only get with a prescription from a healthcare provider. An over-the-counter medicine is one you can buy without a prescription.
It is very important to take your medicines the right way in the days leading up to your procedure. If you don’t, we may need to reschedule your procedure.
Blood thinners
Blood thinners are medications that affect the way your blood clots. If you take blood thinners, ask the healthcare provider performing your procedure what to do. They may recommend you stop taking the medication. This will depend on the type of procedure you’re having and the reason you’re taking blood thinners.
We’ve listed some examples of common blood thinners below. There are others, so be sure your care team knows all the medicines you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
Diabetes medicines
If you take insulin or other diabetes medicines, talk with the healthcare provider doing your procedure and the healthcare provider who prescribes it. Ask them what to do before your procedure. You may need to stop taking it or take a different dose (amount) than usual. You may also need to follow different eating and drinking instructions before your procedure. Follow your healthcare provider’s instructions.
Your care team will check your blood sugar levels during your procedure.
Weight loss medicines
If you take medicine for weight loss (such as a GLP-1 medicine), talk with the healthcare provider doing your procedure. Ask them what to do before your procedure. You may need to stop taking it, follow different eating and drinking instructions before your procedure, or both. Follow your healthcare provider’s instructions.
We’ve listed some examples of medicines that cause weight loss below. There are others, so be sure your care team knows all the medicines you take. Some of these are meant to be used to help manage diabetes but are sometimes prescribed just for weight loss.
|
|
Diuretics (water pills)
A diuretic is a medicine that helps control fluid buildup in your body. Diuretics are often prescribed to help treat hypertension (high blood pressure) or edema (swelling). They can also be prescribed to help treat certain heart or kidney problems.
If you take a diuretic, ask the healthcare provider doing your procedure what to do before your procedure. You may need to stop taking it the day of your procedure.
We’ve listed some examples of common diuretics below. There are others, so be sure your care team knows all the medicines you take.
|
|
Get a letter from your doctor, if needed
If you have an automatic implantable cardioverter-defibrillator (AICD), talk with your cardiologist (heart doctor) about your procedure. You may need to get a clearance letter from them before your procedure. A clearance letter is a letter that says you can have the procedure. Follow your care team’s instructions.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
What to do the day before your rigid bronchoscopy
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your surgery. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their surgery.
What to do the day of your rigid bronchoscopy
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before surgery, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your surgery.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Things to remember
- Follow your healthcare provider’s instructions for taking your medications the morning of your procedure. It’s OK to take them with a few small sips of water.
- Wear loose, comfortable clothing.
- If you wear contact lenses, wear your glasses instead, if you can. If you don’t have glasses, bring a case for your contacts.
- Do not put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne.
- Take off any jewelry, including body piercings.
- Leave all valuable items, such as credit cards and jewelry, at home.
- When it’s time for your procedure, you’ll need to remove your hearing aid(s), dentures, prosthetic device(s), wig, and religious articles.
What to bring
- A list of the medications you take at home, including patches and creams.
- Your rescue inhaler (such as albuterol for asthma), if you have one, or any other medications for breathing.
- Your cell phone and charger.
- Only the money you may want for small purchases, such as a newspaper.
- A case for your personal items, if you have one. This includes glasses or contacts, hearing aid(s), dentures, prosthetic device(s), wig, or religious articles.
- Your Health Care Proxy form and other advance directives, if you have filled them out.
- Your breathing device for sleep apnea (such as your CPAP machine), if you use one. If you can’t bring it, we will give you one to use while you’re in the hospital.
- If you have an implanted pacemaker or automatic implantable cardioverter-defibrillator (AICD), bring your wallet card with you.
Where to go
Your procedure will be done at one of these locations:
Endoscopy suite at Memorial Hospital (the main hospital at MSK)
1275 York Ave. (between East 67th and East 68th streets)
New York, NY 10065
Take the B elevator to the 2nd floor. Turn right and enter the Surgery and Procedural Center through the glass doors.
Operating room at Memorial Hospital (the main hospital at MSK)
1275 York Ave. (between East 67th and East 68th streets)
New York, NY 10065
Take the B elevator to the Presurgical Center (PSC) on the 6th floor.
What to expect when you arrive at the hospital
Many doctors, nurses, and other staff members will ask you to state and spell your name and date of birth. This is for your safety. People with the same or similar names may be having procedures on the same day.
When it’s time to change for your procedure, you’ll get a hospital gown and nonskid socks to wear. You’ll be asked to remove your glasses or contacts, hearing aid(s), dentures, prosthetic device(s), wig, or religious articles, if you have any.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicine, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
The IV will be used to give you anesthesia (medication to make you sleep) during your procedure. You may also get fluids through the IV before your procedure.
Meet with an anesthesiologist
You will also meet with an anesthesiologist (A-nes-THEE-zee-AH-loh-jist). An anesthesiologist is a doctor with special training in anesthesia. They will give you anesthesia during your procedure. They will also:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your procedure.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Meet with your doctor
You’ll talk with your doctor before your procedure. They will explain the procedure and answer your questions.
What to expect during your rigid bronchoscopy
When it’s time for your procedure, you’ll go into the procedure room and be helped onto an exam table. Your healthcare provider will set up equipment to monitor your heart rate, breathing, and blood pressure. You’ll also get oxygen through a thin tube that rests below your nose.
Then, you’ll get anesthesia through your IV line. Once you’re asleep, your doctor will insert (put) the bronchoscope into your mouth. They will gently move it down the back of your throat and through the airways leading into your lungs (see Figure 1).
Your doctor may use a laser, electrocautery (electricity), or cryotherapy. This will heat, burn, or freeze the tumor or areas of bleeding inside your airways. They may use fluoroscopy (live X-ray) during your procedure to guide them.
Your doctor may also place a stent inside your airway to help keep it open.
The rigid bronchoscopy usually takes about 60 to 90 minutes.
What to expect after your rigid bronchoscopy
In the Post-Anesthesia Care Unit (PACU)
When you wake up after your procedure, you’ll be in the Post-Anesthesia Care Unit (PACU).
A nurse will keep track of your body temperature, pulse, blood pressure, and oxygen levels. You may feel numbness in your throat. This is from medication used to make you more comfortable and reduce coughing. The numbness will go away shortly after you wake up.
You may have a chest X-ray to make sure your lung was not damaged. This type of injury is rare.
Once you’re fully awake, your nurse may give you a drink and a light snack. They will also take out your IV. Your doctor will talk with you and the person taking you home about how your procedure went.
If you stopped taking any medications before your procedure, ask your doctor when you can start taking them again.
Before you leave, your nurse will explain your discharge instructions to you and the person taking you home. If you had a stent placed, you’ll get instructions on how to take care of it.
At home
-
After your procedure, you may have none, some, or all of these side effects:
- A sore throat.
- A low-grade fever (below 101 °F or 38.3 °C).
- Coughing up a small amount of blood.
These side effects should go away within 3 days. Eating soft foods and sucking on ice chips or throat lozenges may help your sore throat. Avoid eating spicy foods and smoking.
- You may cough up streaks of blood. This is normal after having this procedure. If you cough up more than 1 teaspoon of blood, call your healthcare provider’s office.
- You can go back to doing your usual activities after your procedure.
- A nurse will call you the day after your procedure to ask how you’re doing.
-
If tests were done during your rigid bronchoscopy, call your healthcare provider’s office in a few days to get the results.
- If you have an MSK MyChart account, you’ll be able to see your test results as soon as they’re available. You may see them before your healthcare provider does. While some results are easy to understand, others may be confusing or worrying. You can choose to look at your results, but we recommend waiting until you talk with your healthcare provider. They can explain what your results mean.
- If you need any more equipment, such as nebulizer, it will be ordered through your healthcare provider’s office.
When to call your healthcare provider
Call your healthcare provider if you:
- Have a fever of 101 °F (38.3 °C) or higher.
- Have trouble breathing or shortness of breath.
- Have chest pain or a feeling of pressure in your chest.
-
Cough up:
- More than 1 teaspoon of blood.
- Any amount of blood for more than 3 days after your procedure.
- Have very bad pain or pain that lasts more than 2 days.
