This information explains how to use the gravity method to feed yourself through your feeding tube.
You may have a feeding tube with a legacy connector or an ENFit connector. In this resource, we will show images of both types of connectors.
About tube feeding with the gravity method
The gravity method is a way to send formula from your feeding bag and into your feeding tube by the force of gravity. Gravity pulls the formula in a downward direction through your feeding tube.
For more information about your feeding tube, including how to manage side effects, read Tube Feeding Troubleshooting Guide.
Tube feeding goals
Your clinical dietitian-nutritionist will talk with you about your daily nutrition and hydration goals. You will also need to flush your feeding tube to clean it and keep you hydrated. Flushing your feeding tube means to gently push water through it. Your healthcare provider will tell you how many times to do this.
How to use the gravity method during your tube feeding
Follow the steps in this section during your tube feeding. Read How to Prevent Aspiration to learn how to avoid having your formula go down your airway.
-
Clean your hands.
- If you’re washing your hands with soap and water, wet your hands, apply soap, rub them together thoroughly for at least 20 seconds, then rinse. Dry your hands with a towel. Use that same towel to turn off the faucet.
- If you’re using an alcohol-based hand sanitizer, cover your hands with it. Rub your hands together until they’re dry.
-
Gather your supplies in a clean and comfortable place. Do not set up or do your tube feeding in the bathroom. You will need:
- The amount of formula prescribed by your healthcare provider.
- A gravity feeding bag.
- A cup.
- An IV pole or hook for hanging the feeding bag.
- A clean cloth or paper towel.
- A container of water. You can use tap water at room temperature as long as it’s safe to drink.
- A 60 milliliter (mL) legacy catheter tip or ENFit syringe.
- A clean cloth or paper towel.
- Tape.
-
A button adapter, if you have a button instead of a tube (see Figures 1 and 2).
- If you’re admitted to the hospital, bring your button adapter with you, if you have one.

Figure 1.
Button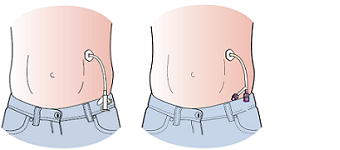
Figure 2. Tube with legacy connector (left) and ENFit (right)
- If you’re admitted to the hospital, bring your button adapter with you, if you have one.
-
Close the roller clamp on the feeding bag (see Figure 3).
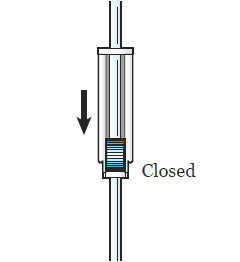
Figure 3. Close the roller clamp -
Wipe the top of the formula can with a clean cloth or paper towel. Pour the prescribed amount of formula into the feeding bag (see Figure 4).
-
The bag will only hold 1,000 mL (4 cans) at a time. If you run the feeding throughout the day or night, pour in 6 to 8 hours worth of formula per feeding at a time. For example, if your tube feeding rate is 120 mL per hour, then pour 1 can every 2 hours. You can fill the bag with 3 to 4 cans at a time.
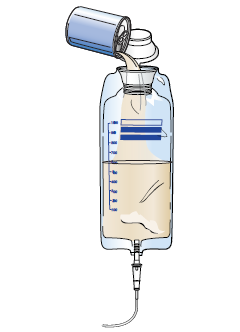
Figure 4. Fill the feeding bag
-
The bag will only hold 1,000 mL (4 cans) at a time. If you run the feeding throughout the day or night, pour in 6 to 8 hours worth of formula per feeding at a time. For example, if your tube feeding rate is 120 mL per hour, then pour 1 can every 2 hours. You can fill the bag with 3 to 4 cans at a time.
-
Hang the feeding bag 2 to 3 feet (.6 to .9 meters) above you on either an IV pole or hook (see Figure 5). It should be close to a comfortable chair or your bed.

Figure 5. Hang the feeding bag - Hold the end of the feeding bag tube over a cup. Remove the cap at the end of the tube.
-
Slowly open the roller clamp on the feeding bag tube (see Figure 6). Let the formula run through the tubing, then close the clamp. This gets the air out of the tubing.
-
If your feeding bag tubing does not have a roller clamp, slowly open the cap, and pinch the tubing until the liquid gets to the end.

Figure 6. Open roller clamp
-
If your feeding bag tubing does not have a roller clamp, slowly open the cap, and pinch the tubing until the liquid gets to the end.
-
Open the plug at the end of your feeding tube (see Figure 7). If you have a button, put the adapter into it (see Figure 8).
- If you’re using a tube without a clamp, pinch the end of the tube to avoid leakage or put the tube in a cup.
-
For the rest of this resource, when we use the words “unclamp” or “reclamp,” you should “unpinch” or “repinch” your feeding tube instead.
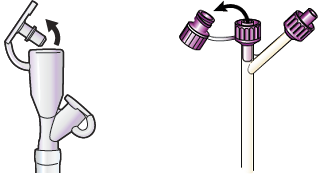
Figure 7. Open plug at end of legacy connector (left) and ENFit (right) 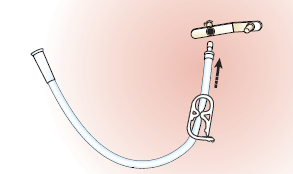
Figure 8. Put adapter
into button
- Fill the syringe with the amount of water recommended by your healthcare provider. Place the syringe into the end of your feeding tube or button adapter.
-
Unclamp your feeding tube (see Figure 9). Flush your feeding tube (see Figure 10).
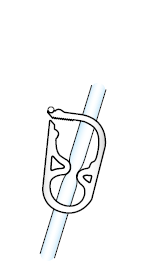
Figure 9.
Unclamp your
feeding tube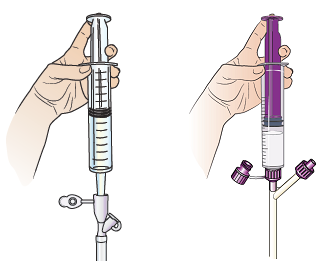
Figure 10. Flush your feeding tube with
legacy connector (left)
and ENFit (right) - Reclamp your feeding tube. Disconnect the syringe.
-
Connect the end of the feeding bag tubing to your feeding tube or button adapter (see Figure 11). Make sure that the end of the tube is placed firmly. You can put a piece of tape over the connection to keep it from separating.
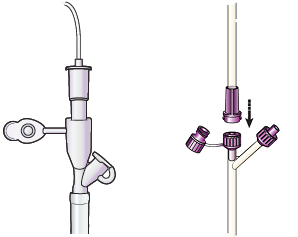
Figure 11. Connect feeding bag tubing to feeding tube with legacy connector (left) and ENFit (right) -
Unclamp your feeding tube and slowly open the roller clamp on the feeding bag tubing (see Figure 12). Allow the formula to drip in over at least 30 minutes.
- Check the bag every 5 to 10 minutes. If the formula is flowing too fast or too slowly, adjust the roller clamp as needed.
-
You can also lower or raise the bag to change the flow of the formula. As you do this more and more, you’ll will learn how high to hang the bag.
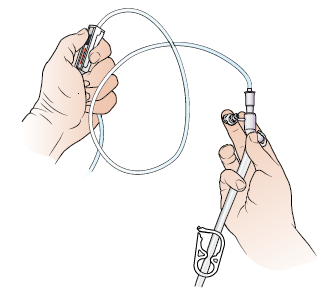
Figure 12. Unclamp feeding tube and open roller clamp
- When the feeding bag is empty, close the roller clamp on the feeding bag tubing. Close the clamp on your feeding tube. Disconnect the feeding bag and set it aside.
-
Fill the syringe with the amount of water recommended by your healthcare provider. Place the syringe into the end of your feeding tube or button adapter. Unclamp and flush your feeding tube.
- Use a new syringe every 24 to 48 hours (1 to 2 days) to prevent infection.
- Clamp your feeding tube, remove the button adapter (if you’re using one), and cap your feeding tube.
-
When you’re done, rinse the feeding bag. Pull the pieces of the syringe apart and rinse each part with warm water. Let your supplies air dry.
- Use a new feeding bag every 24 to 48 hours (1 to 2 days) to prevent infection.
Repeat steps 1 to 17 with each feeding.
How to connect and disconnect your extension set from your MIC-KEY button adaptor
If you have a button adaptor, follow these steps to connect and disconnect your tubing from the button:
- Uncap the button (or MIC-KEY feeding port).
- Place the extension set over the button.
-
Line up the black lines on the extension set and the button and push down firmly.
- To connect, follow the arrow on the adapter by turning it clockwise (to the right) until it locks in place. Do not turn the connector past the lock place. Keep the extension in this locked position during feeding.
- To disconnect, follow the arrow on the adapter by turning it counterclockwise (to the left) until the black lines line up. Pull the adapter up.
Points to remember when using your feeding tube
- Use a new syringe every 1 to 2 days to prevent infection.
- Use a new feeding bag every 1 to 2 days to prevent infection.
- Always reclamp your feeding tube before removing your legacy catheter tip or ENFit syringe to avoid leakage.
- Move the clamp to different sections of your feeding tube to avoid permanently kinking or bending the tube.
-
To avoid clogging, always flush your feeding tube with the amount of water recommended by your healthcare provider (usually 60 mL) before and after:
- Each feeding.
- Taking each medication.
- If you’re not using your feeding tube daily, flush it with 60 mL of water at least once a day. This will keep the feeding tube from getting clogged.
- If you’re taking medications with your feeding tube in place, read How to Take Medications Through Your Feeding Tube.
How to order supplies
Your case manager will check with your insurance company about your insurance coverage. If your insurance covers tube feedings, we will refer you to a home care provider. They’ll give you formula and equipment. Always reorder formula and equipment when you have at least 10 days of supplies at home. This will help you make sure you never run out of formula.
If your insurance does not cover your formula or supplies, you can buy that brand or a generic version at your local pharmacy, grocery store, or online. Talk with your healthcare provider about what generic version is right for you.
If you’re no longer using a feeding tube, you can donate your leftover supplies. Contact the Oley Foundation by calling 518-262-5079 or visit their website at www.oley.org
How to store your formula
- Check the expiration date of your formula. Unopened cans of formula can be stored at room temperature for long periods of time.
- Cover open cans of formula and store them in the refrigerator between feedings. Throw away any open, unused cans of formula after 24 hours.
When to call your healthcare provider
Call your healthcare provider if you:
-
See any of the following at your insertion site:
- Bleeding that soaks a small gauze pad.
- Pus or drainage that smells bad.
- Redness.
- Swelling.
- Increased pain that does not go away with medication.
-
Have any of the following changes to your bowel function:
- Haven’t had a bowel movement (pooped) in 2 days.
- Have hard and dry bowel movements.
- Have any changes in your bowel movement, such as in the color, consistency, frequency, or amount.
- Have any changes in your urine (pee), such as in the color, frequency, or amount.
-
Have changes in your weight, such as:
- Gain more than 5 pounds (2.3 kilograms) per week.
- Lose more than 2 pounds (0.90 kilograms) per week.
- Feel too full after tube feeding.
- Have swelling in your abdomen (belly), feet, legs, hands, or face.
- Have nausea (feeling like you’re going to throw up).
- Are vomiting (throwing up).
- Have bloating, stomach cramps, or diarrhea (loose or water bowel movements).
- Have a fever of 100.4° F (38° C) or higher.
- Have chills.
- Are dizzy.
- Have trouble breathing.
