This information will help you understand your family member or friend’s pancreaticoduodenectomy (PAN-kree-uh-koh-DOO-ah-deh-NEK-toh-mee), also called a Whipple procedure. The Whipple procedure is a surgery to remove a tumor in the head of the pancreas. Use this guide as a reference while you wait during the surgery and when getting updates from your nurse liaison.
About the organs in the digestive system
Pancreas
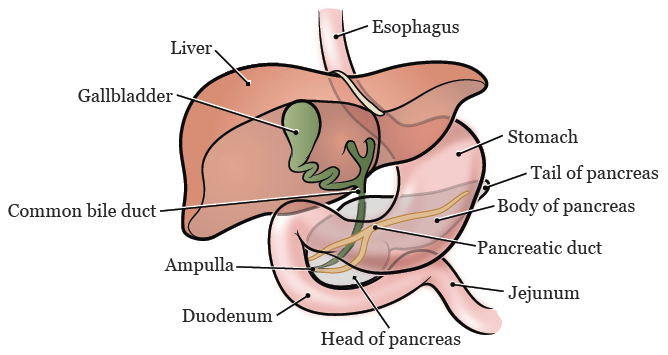
The pancreas is in the back of the abdomen (belly). It sits behind the stomach and just above the small intestine (see Figure 1). The pancreas has 3 sections: the head, body, and tail. The head of the pancreas is attached to the duodenum (the first part of the small intestine).
The pancreas has 2 main functions:
- Make digestive fluids that help break down fats and proteins.
- Make insulin and glucagon. These are hormones that help control blood glucose (sugar) levels.
Common bile duct
The common bile duct is a small tube. It moves bile from the liver to the gallbladder to be stored, then from the gallbladder into the duodenum. Bile is made in the liver and helps the body digest fat.
Gallbladder
The gallbladder is a small, tear-drop shaped organ located under the liver. Its main job is to store bile. When you eat food, the gallbladder sends stored bile to the duodenum to help with digestion.
Duodenum
The duodenum (DOO-ah-DEE-num) is the first part of the small intestine. It’s directly attached to the stomach. Partially digested food moves from the stomach into the duodenum. There, the food is further digested by bile from the gallbladder and digestive fluids from the pancreas.
Jejunum
The jejunum (jeh-JYOO-num) is the middle part of the small intestine. Digestion continues here.
About the Whipple procedure
The Whipple procedure is a surgery to remove a tumor in the head of the pancreas. It can be done using different techniques. The surgeon will talk with the person about which one is right for them. Depending on the type of surgery they have, the surgeon will make 1 or more incisions (surgical cuts).
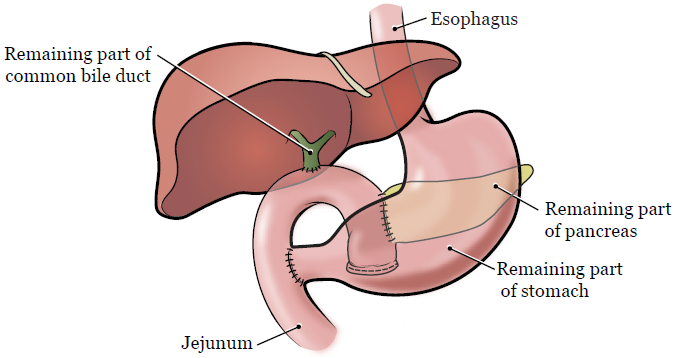
During a Whipple procedure, the surgeon will remove:
- The gallbladder.
- The head of the pancreas.
- The duodenum.
- The end of the common bile duct.
- Sometimes, they must also remove part of the stomach.
Then, the surgeon will connect the remaining parts of the common bile duct, pancreas (tail), and stomach to the jejunum. This lets pancreatic fluids and bile flow into the small intestine the way they did before (see Figure 2). There’s usually enough left of the pancreas after surgery to keep making digestive fluids and hormones.
What to expect when you arrive
Many staff members will ask the person to say and spell their name and birth date. This is for their safety. People with the same or similar names may be having a procedure on the same day.
When it’s time to change, they’ll get a hospital gown, robe, surgical head covering, and nonskid socks to wear.
Once the person is checked in, they will go to the Presurgical Unit to be examined before surgery.
Sometimes, surgeries are delayed. This could happen if an earlier surgery takes longer than expected or for other reasons beyond our control. We will make every effort to tell you if that happens.
When the operating room (OR) is ready, the surgical team will take the person there. They will get them ready for surgery. This can take 15 to 90 minutes.
The nurse liaison role
A nurse liaison is a nurse who communicates with patients, family and friends, and the care team.
Sometimes, the surgeon will need to speak with the person’s family and friends during the surgery. They may need to talk about what they see during surgery. If this happens, the nurse liaison will be there for the conversation.
Contact the nurse liaison if a problem comes up or if you just need to talk. If you’re at the hospital, ask a staff member at the front desk to contact the nurse liaison for you. To reach your nurse liaison from outside of the hospital, call 212-639-2000 and ask for beeper 9000.
During surgery
The surgery usually takes about 4 hours, but this may vary. The nurse liaison will call you every 2 hours with updates throughout the surgery.
After surgery
A member of the care team will call you when the surgery is almost finished. The surgeon will explain what they found during the surgery. You will be able to ask them questions.
After surgery, a staff member will take the person to the post-anesthesia care unit (PACU). The person may be tired, groggy, or uncomfortable after surgery.
In the PACU, they will get oxygen through a thin tube that rests beneath their nose. They may be connected to other tubes and wires, such as an intravenous (IV) line to give them pain medication. They may also be connected and a pulse oximeter to measure their oxygen level and heart rate.
The PACU nurse will explain the plan of care for the person. This includes whether the person will stay in the hospital overnight and when they will move to an inpatient room.
We will give you a card with the PACU phone number. Please choose just one person to call for updates.
More resources
Information for Family and Friends for the Day of Surgery
Pancreatic Cancer Action Network
www.pancan.org
877-573-9971
A national patient advocacy organization for the pancreatic cancer community. This organization helps patients and caregivers find information about pancreatic cancer, clinical trials, and support resources. It also has a survivor and caregiver support network.
