Update: On August 19, 2021, the US Food and Drug Administration approved nivolumab for patients with bladder cancer who are at high risk of recurrence following surgery to remove the bladder.
People whose bladder cancer has spread into the muscle wall may soon have a new treatment option after surgery that will help keep the cancer from returning. A large, international clinical trial showed that the immunotherapy drug nivolumab (Opdivo®) is effective at reducing bladder cancer recurrence.
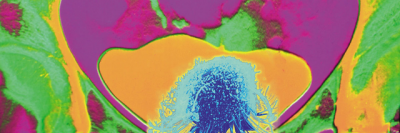
About 25% of bladder cancers fall into this high-risk category, in which the disease is much more likely to spread and is harder to treat. Bladder cancer is the fourth most common cancer in men in the US, and although cases are going down, death rates — in men at least — have been stable.
Memorial Sloan Kettering medical oncologist Dean Bajorin, who played a leading role in the clinical trial, answered questions about the study and how this treatment will benefit many people with bladder cancer.
What is the evidence this new treatment could be effective?
The phase III trial, which involved 709 patients, showed that people who received nivolumab stayed free of cancer — what we call disease-free survival — about twice as long as people who received a placebo. Those who received nivolumab had disease-free survival of 21 months compared with 10.9 months in people receiving the placebo. On behalf of the worldwide investigators on this study, I presented these results in February 2021 at the annual Genitourinary Symposium of the American Society of Clinical Oncology.
The global clinical trial, called CheckMate 274, looked at whether nivolumab could reduce the risk of any urothelial cancer returning in people after they had surgery to remove the bladder, ureter, or kidney. Urothelial cancers are tumors that start in the lining of the urine-collecting system that transports urine from the kidneys to the outside of our bodies. These cancers are often referred to as “bladder cancer” because most of them start in the bladder. People in the study had cancer with a very high risk of recurrence despite surgery — both a high (aggressive) grade of tumor and a cancer that grew into the muscle layer of the bladder, ureter, or kidney. They may or may not have had chemotherapy before surgery.
How could this change treatment for bladder cancer patients?
It’s a major advance. The standard of care for these patients has been observation because no chemotherapy or immunotherapy has shown a benefit. A few years ago, another immunotherapy drug, atezolizumab, was tested in an international trial on the same kind of patients and had disappointing results. So, the absence of good treatment options has been frustrating for both patients and doctors — to know someone has high-risk disease and yet not be able to offer them a treatment to reduce recurrence. Now for the first time, a new immunotherapy accomplishes exactly that.
It’s too early to know whether nivolumab will also allow these patients to live longer. This was a double-blinded study, meaning neither doctor nor patient knows who received the drug, and it will take a while longer to learn about the impact on survival. But it’s important not to be focused only on survival and overlook that patients truly benefit by preventing or delaying the cancer’s return. This type of urothelial cancer is an aggressive disease no matter where it starts. When it recurs, patients suffer a serious drop in quality of life, and it impairs their functional ability. So, disease-free survival is very important in its own right. It’s also important to note the vast majority of patients taking the drug still had a high quality of life without serious side effects, which were monitored very closely during the trial.
The trial demonstrates that novel therapies can be identified as having patient benefit when the studies are conducted in a very rigorous fashion. We are hoping this treatment will get approval for all patients at high risk of recurrence after the US Food and Drug Administration has done a detailed review of all the data.
What has been MSK’s contribution to this trial and bladder cancer research?
I was one of the lead investigators in designing this trial, and MSK was one of the sites enrolling patients in this multicenter study. Doing a randomized, double-blind trial with a control group receiving a placebo is very challenging and takes a long time. But it provides very solid results that you can be confident are significant.
MSK has been a leader in bladder cancer research, especially in the use of therapies before and after surgery for muscle-invasive disease. In 2018, the National Cancer Institute awarded MSK a prestigious SPORE grant for bladder cancer research. This grant is overseen in tandem by myself and medical oncologist David Solit. One project, led by medical oncologist Jonathan Rosenberg, seeks to understand what exactly causes urothelial cancer to respond to or resist immunotherapy drugs. We hope this research can lead to more successful clinical trials like CheckMate 274.
Another project, led by Dr. Solit and medical oncologist Gopa Iyer, investigates whether people with muscle-invasive bladder cancer can avoid having their bladders removed. Some people have bladder tumors with genetic changes called DNA-damage response (DDR) mutations. Research has shown that these people usually respond especially well to chemotherapy before surgery.
In a third project, medical oncologist Kenneth Offit, an expert in genetics, is examining patients and their family members for genes that make it more likely to get urothelial cancer in the first place, very similar to the BRCA gene in patients with breast cancer.
MSK has many experts in genetics, molecular oncology, and immunology who can work closely to produce insights that can advance the field. We plan to continue improving the outlook for many people with this disease.