Very early on in the development of the immunotherapy drugs called checkpoint inhibitors doctors realized that melanoma and lung cancer have something important in common. These cancers were the first shown to respond to checkpoint inhibitors. Both tend to have a lot of DNA mutations. Tumors with an elevated number of mutations are referred to as having a high tumor mutational burden (TMB).
Researchers from Memorial Sloan Kettering have conducted a wide-ranging study to find out if the relationship between high TMB and a positive response to checkpoint inhibitor drugs holds across other cancers. Their findings were recently published in Nature Genetics.
“Based on observations in lung cancer and melanoma, experts in the field have made the assumption that the association between mutation burden and immunotherapy response is true for all cancers,” says surgeon-scientist Luc Morris, one of the three senior authors on the paper. “Until now, however, it hasn’t been well studied. Our study asked if TMB has value as a predictive biomarker across all cancers.”

The investigators confirmed that TMB is predictive across many cancer types. They also noted that people with high-TMB tumors who were treated with immunotherapy lived longer compared with those who had high-TMB tumors and got other kinds of treatment. And importantly, they determined that what is considered a high level of TMB varies depending on the type of tumor. This is a critical question that needed to be answered before using this information when caring for patients.
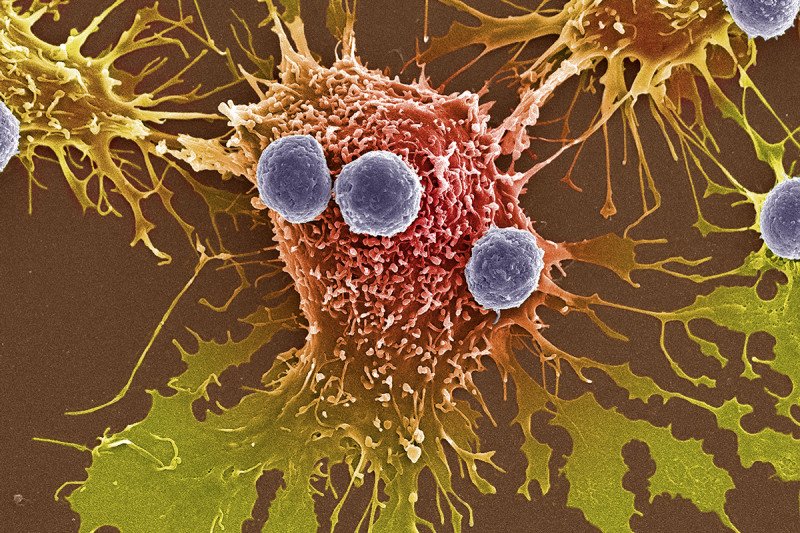
Bringing Tumors Out of Hiding
The relationship between a high TMB and response to immunotherapy was first demonstrated in two groundbreaking studies from MSK researchers. One, published in 2014 by physician-scientists Timothy Chan and Jedd Wolchok, reported the connection in melanoma. Another study the following year from Dr. Chan and then MSK researcher Naiyer Rizvi reported the same relationship between immunotherapy response and high TMB in non-small cell lung cancer.
The connection made sense. DNA mutations lead to the production of altered proteins that the immune system is able to recognize as foreign. The more mutated proteins a tumor has, the more likely it is that the immune system will attack the cancer, and that drugs that promote an immune response, such as checkpoint inhibitors, will be successful in eliminating it.
For melanoma, the high number of mutations results from exposure to the sun’s damaging UV rays. For some lung cancers, bladder cancers, and head and neck cancers — for which immunotherapy drugs often work well — the high TMB may be due to carcinogens in tobacco.
Using Data to Confirm a Long-Standing Assumption
Other cancers also have high TMBs, but these elevated mutation rates tend to appear with less frequency and at varied levels. “The assumption that TMB is a useful predictor of response to checkpoint inhibitors for all types of cancer has not been proven,” Dr. Morris explains. “Until now, we also haven’t known whether this testing is valuable for people who are treated as part of routine care, as opposed to those who were carefully selected for clinical trials.”
The investigators determined that what is considered a high level of TMB varies depending on the type of tumor.
The current study used data from more than 1,600 people who were treated with checkpoint inhibitor drugs at MSK and about 5,300 people who received nonimmune-based treatments. All of the patients had their tumors analyzed with MSK-IMPACT™. The US Food and Drug Administration has authorized this targeted tumor-sequencing assay, which is offered to MSK patients. The test looks for mutations in tumors that can be targeted with drugs and also reports TMB. Results from MSK-IMPACT were anonymously linked with clinical records, allowing researchers to tease out connections between different levels of TMB and drug response.
“The bottom line is that we confirmed that TMB does have predictive value across a range of cancer types,” Dr. Morris says. “We also showed that the predictive value of TMB is dose dependent. This means that the higher the TMB in a person’s cancer, the more likely they are to respond to the drugs.”
But the researchers found that there is not one universal definition for what it means to have a high TMB. For example, having six mutations was considered high in breast cancer and glioblastoma, compared with 31 in melanoma and 52 in colorectal cancer.
A Collaborative Project Focusing on Many Cancer Types
The team was able to conduct such a large, multifaceted project thanks to contributions from 57 researchers from a number of Disease Management Teams. MSK’s Immunogenomics and Precision Oncology Platform (IPOP) and the Marie-Josée and Henry R. Kravis Center for Molecular Oncology (CMO) helped bring together the collaborators and analyze the data.
To further advance this important and growing field of research, all of the data from the study are being made available to other scientists through MSK’s cBioPortal for Cancer Genomics. This will allow scientists at other institutions to use the data to design future trials.
“We are still optimizing the use of TMB as a way to predict response to therapy,” Dr. Morris notes. “We need more research to determine the optimal number of mutations that we should use for each cancer type. We hope that based on our data, researchers will move forward with more clinical studies that will ultimately result in the ability to select the best treatments for people with cancer and allow them to avoid treatments that are unlikely to help them.”
The first author of the Nature Genetics paper is Robert Samstein, a fellow in radiation oncology at MSK. In addition to Dr. Morris, the other senior authors are Dr. Chan, Director of IPOP, and physician-scientist David Solit, Director of the CMO.