The Multidisciplinary Pituitary and Skull Base Tumor Center at Memorial Sloan Kettering Cancer Center brings together doctors from a range of specialties to provide world-class, comprehensive care to patients who have been diagnosed with pituitary, parasellar, paranasal sinus, and other skull base tumors.
We offer a complete array of approaches for treating skull base tumors. When surgery is necessary, we use minimally invasive techniques whenever possible. We perform total tumor removal when appropriate while preserving normal tissue and optimizing quality of life.
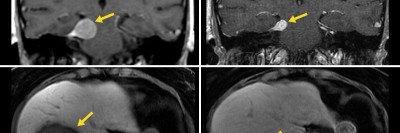
We are one of very few centers in the world that offers intraoperative MRI imaging for every pituitary and skull base tumor surgery. This technology enables our surgeons to view real-time images of a tumor during a procedure, making for a safer and more-effective operation. It also enables us to image patients after a procedure is completed to ensure complete tumor removal while patients are still under anesthesia.
Learn about the many approaches we offer for treating skull based tumors.
Call us on our direct line at 212-639-3935, between and , Eastern time, Monday through Friday.
Upcoming CME: Update on the Treatment of Pituitary Tumors
Friday, April 5, 2024
Providers who treat and manage patients with pituitary diseases, along with patients and caregivers affected by this rare disease, are invited to attend the Update on the Treatment of Pituitary Tumors on Friday, April 5, 2024. This virtual program will provide an update on the latest developments in ongoing basic and translational science and the clinical management of patients with pituitary conditions. Focusing on evidence-based discussions, the course aims to enhance patient care by addressing clinical practice guidelines and emerging therapies, with the goal of advancing early diagnosis and treatment. The multidisciplinary nature of the course facilitates knowledge dissemination among practitioners and patients. The afternoon features two separate tracks dedicated to our clinical/provider and patient/caregiver audiences.
For additional details and registration, please visit: msk.org/PituitaryCourse
Coordinated Care
One of the most important aspects of the center is its multidisciplinary nature. Patients receive personalized care from a team of experts that includes neurosurgeons, head and neck surgeons, endocrinologists, neuro-ophthalmologists, radiation oncologists, medical oncologists, and neuro-radiologists.
Because our team works so closely together, we are able to relieve patients from the burden of coordinating care. For example, someone who needs to see a neurosurgeon, a head and neck surgeon, and a neuro-endocrinologist can do so on the same day at MSK. This approach spares our patients from having to go to multiple appointments over the course of weeks or even months. It also allows us to develop a personalized care plan right away.
- Adenoma
- Cerebrospinal fluid leak
- Clival chordoma
- Craniopharyngioma
- Cushing’s disease
- Encephalocele
- Esthesioneuroblastoma
- Growth hormone secreting tumor
- Juvenile nasopharyngeal angiofibroma
- Macroadenoma
- Microadenoma
- Meningioma
- Meningocele
- Mucocele
- Mucopyocele
- Paranasal sinus tumor
- Pituicytoma
- Pituitary tumor
- Planum meningioma
- Planum sphenoidale tumor
- Proloactinoma
- Rathke’s cleft cyst
- Sinus tumor
- Skull base tumor
- Recurrent nasopharyngeal carcinoma
- Sellar tumor (or lesion or mass)
- Suprasellar tumor (or lesion or mass)
- TSH secreting tumor
Surgical Expertise
Our surgeons are committed to achieving cures while preserving quality of life, and they bring a wealth of technical expertise to each patient’s care. They treat approximately 200 patients with skull base tumors each year and are highly skilled at operating near the delicate structures that surround the base of the skull, such as the optic nerve and carotid artery.
Because these tumors appear at the base of the brain, surgery can often be performed through the nose. New technology has made these procedures safer than ever. MSK surgeons have access to the latest cutting-edge equipment — including high-definition endoscopes, image guidance, and intraoperative MRI — and they have vast experience in operative techniques that minimize side effects.
Transnasal endoscopy involves carefully inserting a small endoscope (a thin, lighted tube with a camera at its tip) through the nasal passage for a magnified view of the skull base. This gives our surgeons a high-definition view of the tumor, which is particularly useful for small tumors buried within the pituitary gland or for larger tumors that have extended into critical areas, such as the optic nerves, the cavernous sinus, or the carotid artery.
Use of a nasoseptal flap is one of several safe, reliable techniques that our surgeons use to separate the brain from the nasal cavity and prevent leakage of cerebral spinal fluid. The approach, which involves using the patient’s own nasal septum tissue, requires no external incision, allowing patients to heal faster with no visible scar. This also ensures that our patients recover with minimal side effects and have normal sinus function after the operation.
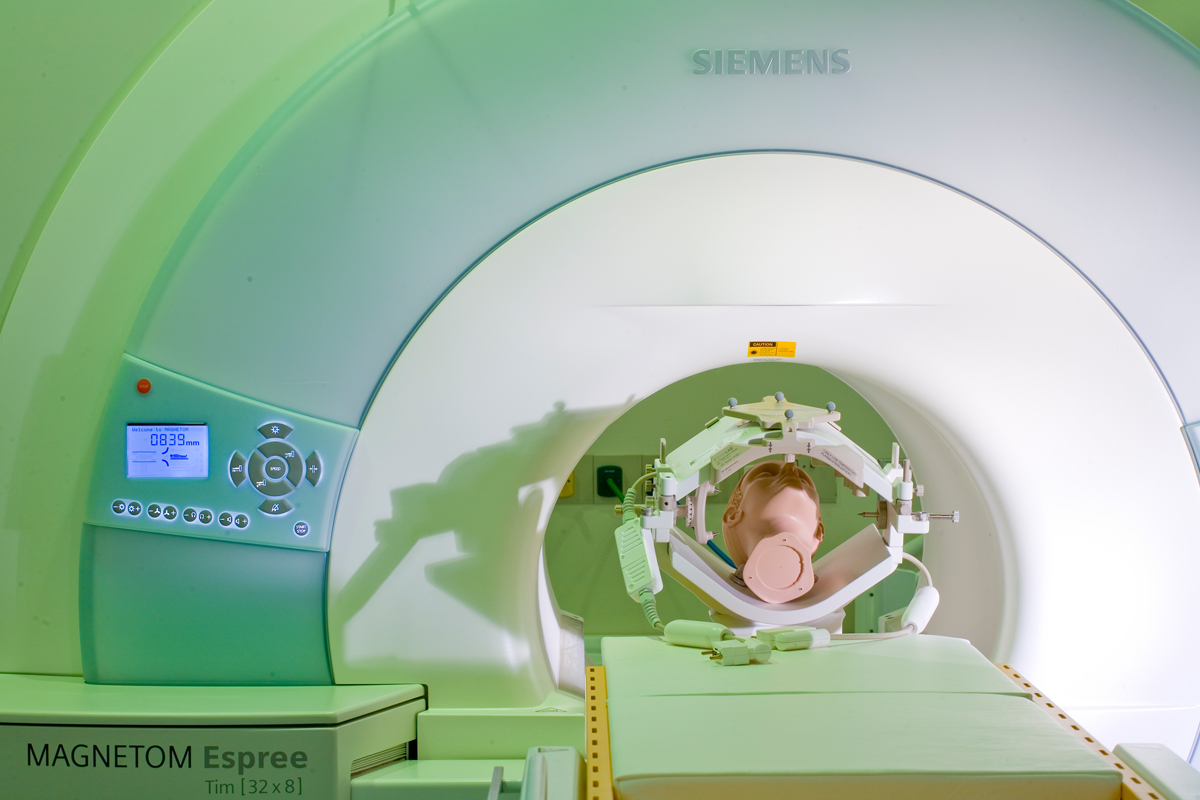
Intraoperative MRI allows our surgeons to view real-time images of a tumor while they’re doing a procedure, making for a safer and more-effective surgery. MSK is one of the few centers in the country to use intraoperative MRI routinely for pituitary and skull base tumors. In addition, MSK is the only center to use intraoperative MRI combined with nasal endoscopic techniques.
In many patients, the optimal treatment for a skull base tumor involves a craniotomy, a surgical procedure in which a section of the skull — called a bone flap — is temporarily removed to access the brain.