For more than three decades, researchers have been thwarted in their attempts to effectively target the cancer-causing effects of the KRAS gene, even as it has been the subject of intensive study. Now a team from Memorial Sloan Kettering has found that a combination of two targeted therapy drugs that are already approved for other types of cancer may halt the growth of lung cancer and pancreatic cancer that carry the KRAS mutation. The study, which was conducted in cell cultures and mice as well as patient samples, was published in June in Nature.
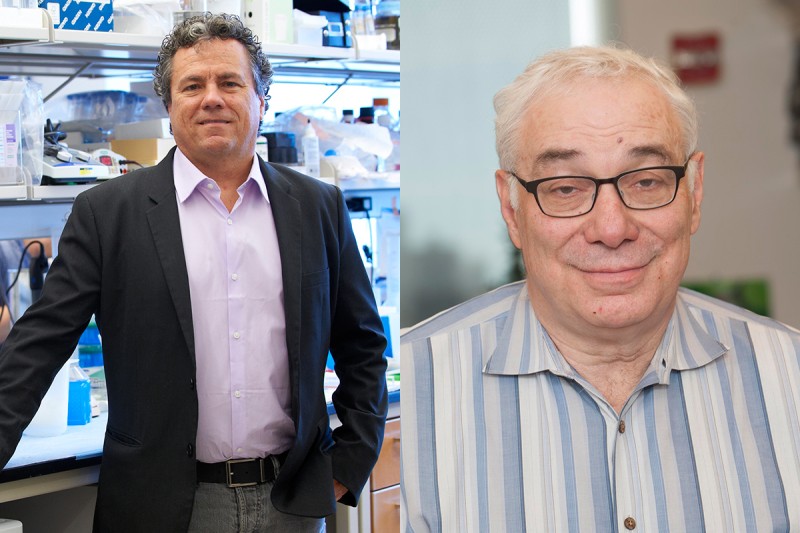
“KRAS is probably the most frequently mutated oncoprotein — meaning that this protein is responsible for driving the growth of many cancers,” says senior author Scott Lowe, Chair of the Cancer Biology and Genetics Program in the Sloan Kettering Institute (SKI) and a Howard Hughes Medical Institute investigator. “A lot of effort has been made to develop small-molecule drugs that block its function on a pharmacological level, but that has proven to be difficult.”
Looking at What Drives Cancer Growth
MSK physician-scientist Neal Rosen, a co-author on the paper and a member of SKI’s Molecular Pharmacology Program, has dedicated many years to studying why blocking mutated Ras function is so challenging. “Activation of oncoproteins causes feedback inhibition of the normal pathways that are used by cells to activate growth,” he says. “Drugs that inhibit the oncoprotein function reactivate these pathways and diminish the anticancer effects of the drugs.” Specifically interfering with the activity of the mutated KRAS protein causes the cell to relieve feedback and find another way to continue growing.
“Think of KRAS mutations like a stuck accelerator on a car, driving the cancer cell to grow,” Dr. Lowe says. “When you use drugs to try to block KRAS action, the cell responds by pushing the accelerator even harder. If you want to short-circuit the cell’s response, you have to not only interfere with the KRAS molecule itself but also blunt the cell’s attempt to compensate.”
Taking a New Approach
The team used a method called functional genomics to determine which other molecules might work in conjunction with KRAS. This approach uses massive amounts of data from gene sequences to determine how genes function and interact with each other. By analyzing KRAS-mutant lung cancer cells in culture that had been treated with a melanoma drug called trametinib (Mekinist®), which acts on part of the KRAS pathway, they found that another molecule, called FGRG1, gets turned on when KRAS is blocked.
“This molecule seemed to fit the theory about the cell’s compensatory response to blocking KRAS, so we decided to see what would happen if we blocked the FGRG1 pathway at the same time,” Dr. Rosen says. They did this with another targeted drug, called ponatinib (Iclusig®), which is used to treat certain types of leukemia.
The researchers studied the combination in several models — cultures of lung cancer and pancreatic cancer cells that were driven by KRAS, as well as several mouse models of these cancers. In all of these, the two-drug combination was effective at killing the cells. They also analyzed biopsy samples from two patients who had been treated with trametinib and showed that the FGRG1 pathway in their tumors was activated, suggesting that their findings could translate to patients.
Based on this work, the team is now planning the first trial to treat patients with KRAS-mutant lung and pancreatic cancer with the drug combination.
Killing Cancer with a Drug Combination
“Until we did the genetic experiments, it wasn’t obvious that combining a melanoma drug with a leukemia drug could be effective against these other cancers,” Dr. Lowe says. “But after we started this research, it was an immediate lightbulb moment that we should take these drugs and mix them together.”
In addition, he says that the functional genomics approach used by his team can serve as a blueprint for other investigators studying complicated cancer-causing pathways in cells. He notes that it also may be useful in finding new drug targets for patients who develop resistance to other targeted therapies like trametinib.
“This is an extension of the idea of precision medicine, where you find a drug that matches with a particular tumor,” Dr. Lowe says. “Ultimately, it will help us to find new drugs as well as point to ways we can repurpose existing drugs for new applications.”